Topics: Peripheral Artery Disease, "Diabetic Foot Disease", Diabetes, diabetic foot ulcer
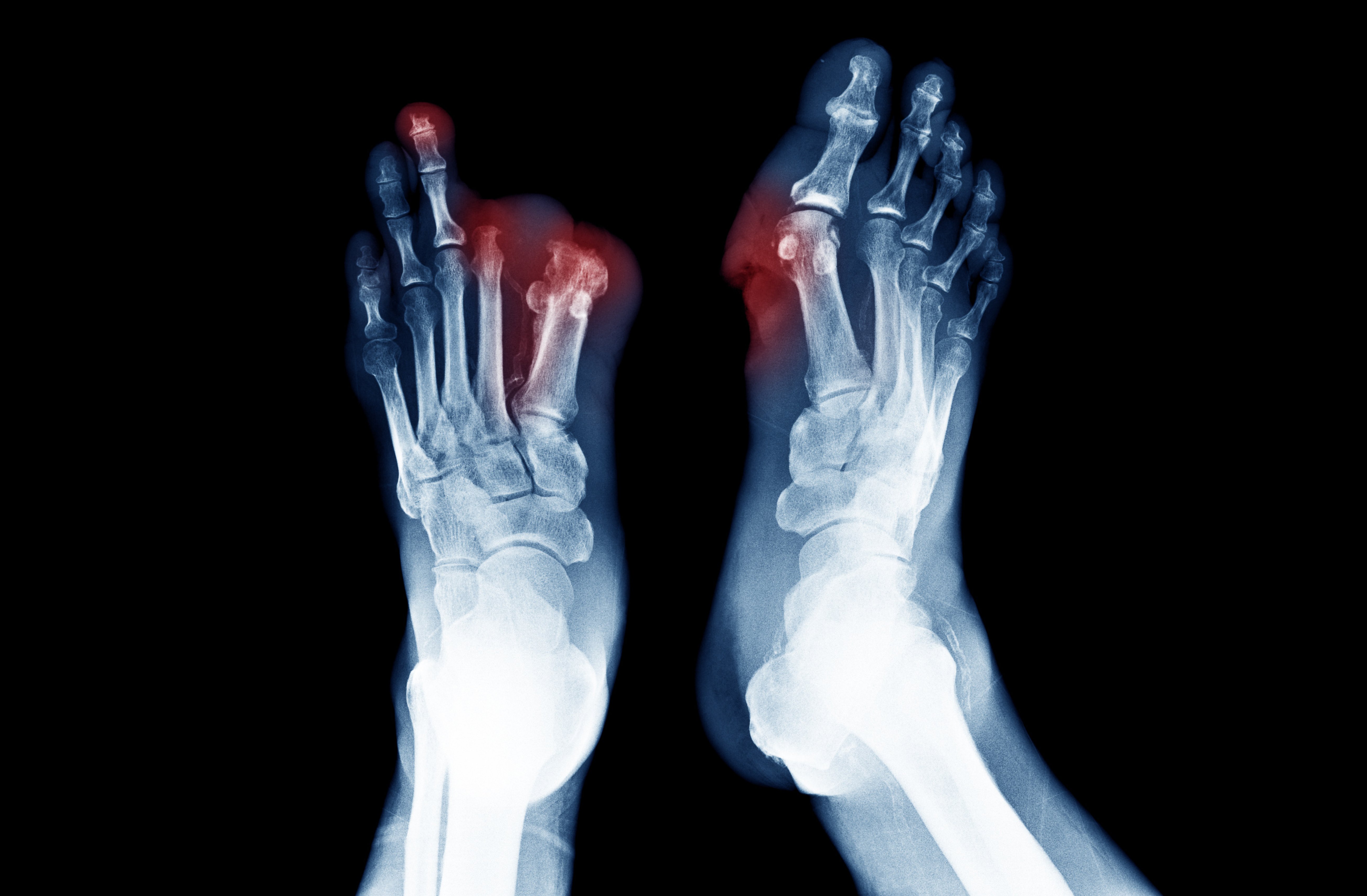
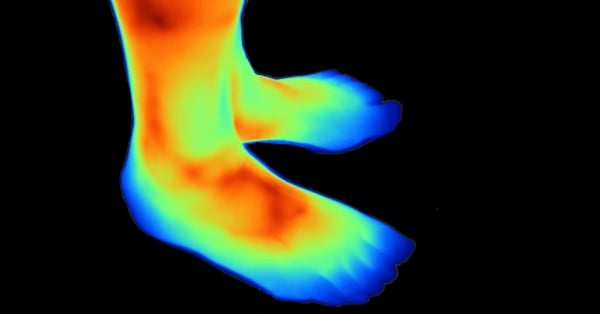
The relationship between diabetes and peripheral artery disease (PAD) is complex. A diabetic foot ulcer requires adequate blood circulation to heal. If the circulation is impaired such that tissue oxygen demand exceeds supply, critical limb ischemia may ensue. A diabetic’s limb can become at risk when antibiotics are unable to reach the infected wound due to clogged arteries.
- 30.3 million Americans are living with diabetes.1
- Up to 40% diabetics have PAD.2
- Up to 25% of those with diabetes will develop ulcers in their lifetime.3
- 50% mortality rate at two years for individuals with diabetes and PAD.2
- 25% of foot ulcers will not heal.2
- 85% of diabetes-related lower extremity amputations are preceded by a foot ulcer.4
- Lower-limb ulcers are the most reliable harbingers of future amputation.5
- Every year, >1 million diabetics suffer limb loss.6
- Every 20 seconds, an amputation occurs in the world due to diabetes.5,6
- 28% of foot ulcers may result in some form of amputation.2
- Foot ulcers and amputations cost the U.S. health care system an estimated $29 billion in 2007.7
- Revascularization should be strongly considered if a diabetic foot wound does not promptly respond to standard wound care.2
- Diabetics with lower extremity complications have 5-year mortality rates similar or worse than many common types of cancer.8
Conclusion:
If you are suffering from diabetic foot disease and your wounds are not healing, blocked arteries due to PAD might be the culprit. Treatment guidelines state that a revascularization procedure “should be strongly considered if a diabetic foot wound does not promptly respond to standard wound care.”2
Treating the infection with antibiotics requires adequate blood flow to infected tissues.8 For this reason, a procedure to unclog the arteries can be vital to saving the limb.9
A revascularization procedure, such as Lumivascular atherectomy, works by removing plaque from your arteries and restoring blood flow to your lower limbs. A significant advancement in the treatment of patients with peripheral artery disease and diabetes is image-guided atherectomy with Lumivascular technology. This minimally invasive procedure allows a doctor to see inside an artery so that they can precisely remove plaque that is preventing blood flow. In addition, a Lumivascular procedure helps prevent against vessel injury which has been shown to cause the return of blockage within a year.10
To find a doctor in your area offering a Lumivascular atherectomy, click here.
Learn more:
About a Lumivascular atherectomy
Find a Lumivascular physician in your area, click here.
If you have found this article helpful, please don’t forget to share!
References:
- Center for Disease Control and Prevention. (July 18, 2017) New CDC report: More than 100 million Americans have diabetes or prediabetes. Retrieved from: https://www.cdc.gov/media/releases/2017/p0718-diabetes-report.html
- Hingorani, et al. The management of diabetic foot: A clinical practice guideline by the Society for Vascular Surgery in collaboration with the American Podiatric Medical Association and the Society for Vascular Medicine. J Vasc Surg 2016;63:3S-21S
- Singh, et al. Preventing foot ulcers in patients with diabetes. JAMA 2005;293:217-28.
- Pecoraro, et al. Pathways to diabetic limb amputation: basis for prevention. Diabetes Care 1990;13:513-21.
- Beckert, et al. A New Wound-Based Severity Score for Diabetic Foot Ulcers. Diabetes Care 2006; 29:988–992
- Boulton, et al. J. The global burden of diabetic foot disease. Lancet 2005;366:1719-24.
- Rogers, et al. The right to bear legs—An amendment to healthcare; how preventing amputations can save billions to the US health-care system. J Am Podiatr Med Assoc 2008;98:166-8.
- Armstrong, et al. Guest editorial: are diabetes-related wounds and amputations worse than cancer? Int Wound J. 2007;4(4):286–7
- Schaper, et al. Specific guidelines for the diagnosis and treatment of peripheral arterial disease in a patient with diabetes and ulceration of the foot 2011. Diabetes Metab Res Rev 2012; 28(Suppl 1): 236–237
- Tarricone, et al. Histopathological Evidence of Adventitial or Medial Injury Is a Strong Predictor of Restenosis During Directional Atherectomy for Peripheral Artery Disease. J Endovasc Ther. 2015 Oct;22(5):712-5.