Topics: Peripheral Artery Disease, Atherectomy, Diabetes, Leg pain, Amputation, PAD Awareness Month, PAD Diagnosis, PAD, sleep
As the curtain lowers on PAD Awareness Month, we find ourselves at a pivotal juncture in the battle against Peripheral Artery Disease (PAD). This annual observance serves as a reminder of the urgency surrounding this often underestimated condition. In 2023, PAD continues to exert its impact on global health, affecting millions of lives and challenging healthcare professionals and researchers alike. As we conclude this month dedicated to awareness, education, and action, let's take a comprehensive look at the current state of Peripheral Artery Disease—its prevalence, advancements in understanding and treatment, and the empowering steps individuals can take to prevent its onset. Join us in exploring the landscape of PAD and its potential for transformation in the years ahead.
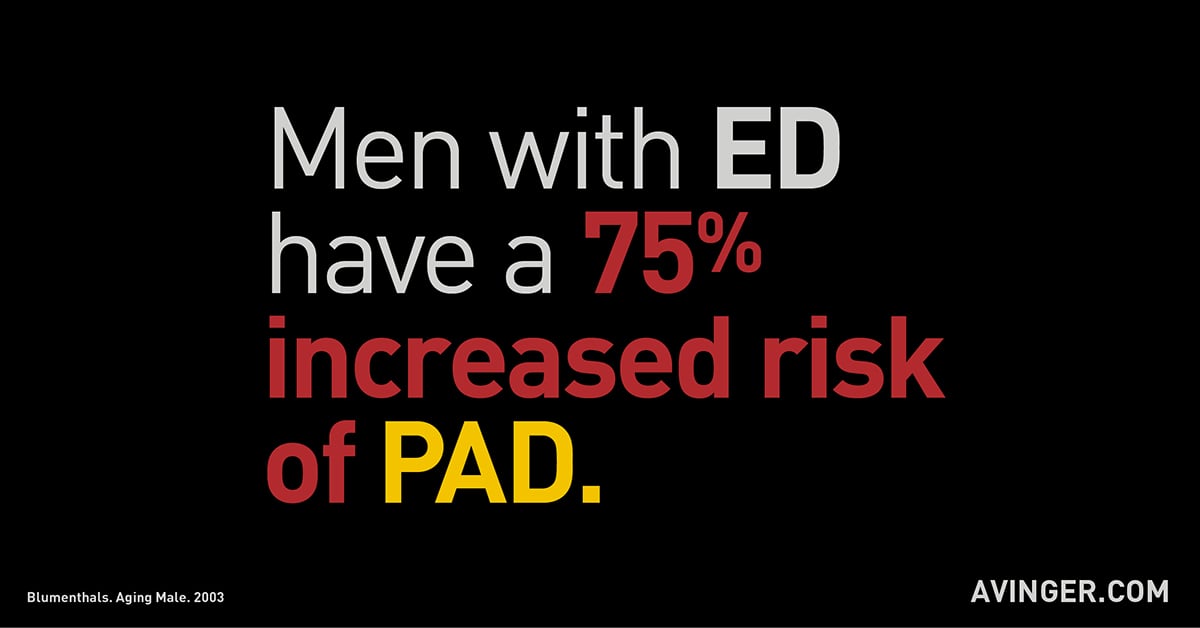
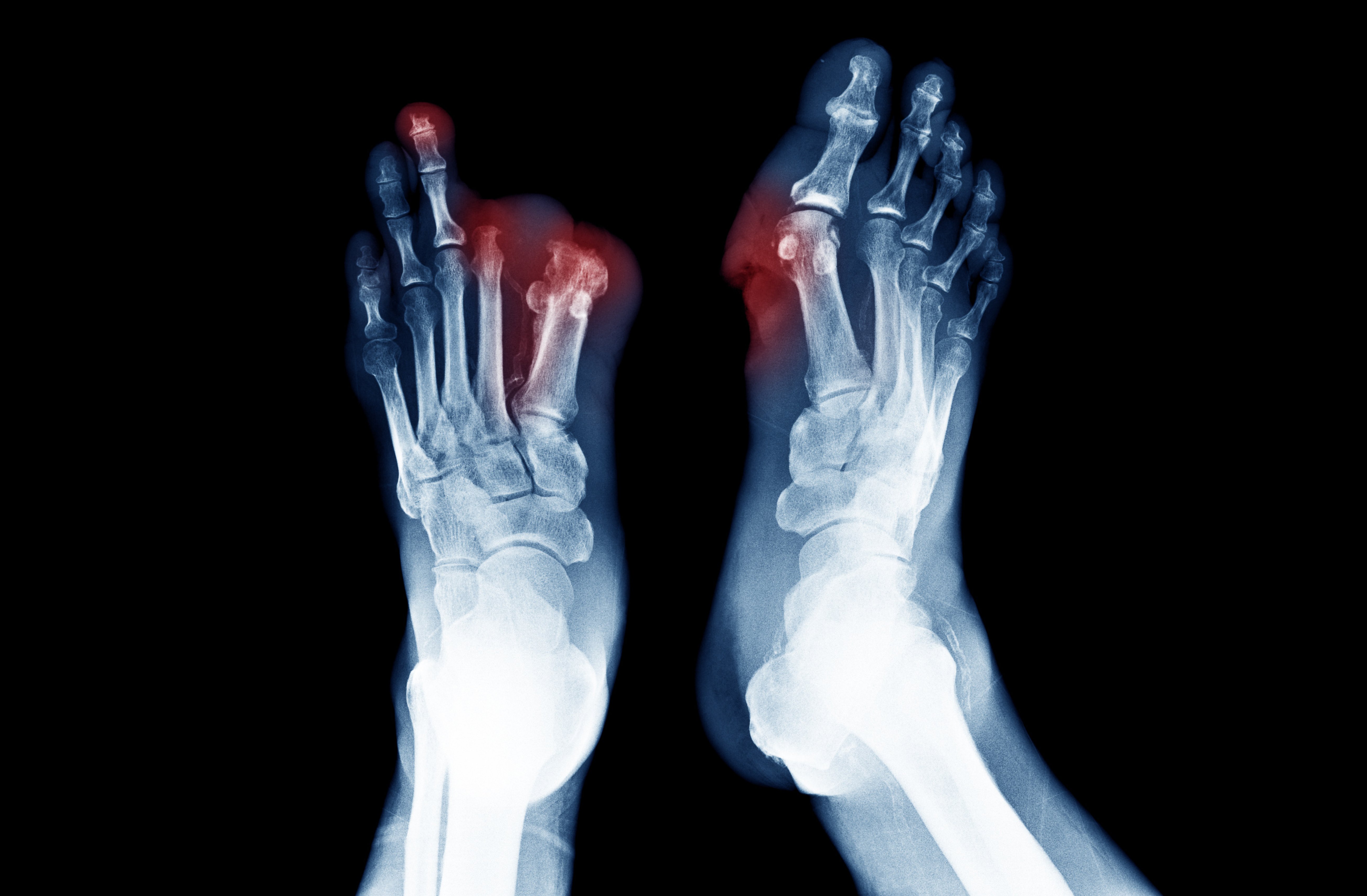
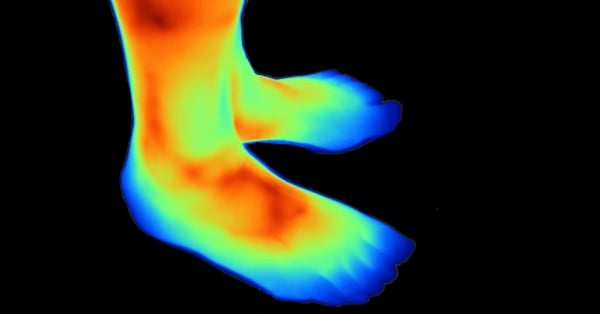
At its core, PAD is a circulatory condition characterized by the narrowing of arteries that supply blood to the extremities, most commonly the legs. This narrowing, often caused by the accumulation of fatty deposits within the arteries, restricts blood flow, leading to a range of symptoms including leg pain, numbness, and even non-healing wounds. As PAD silently affects millions around the world, it simultaneously presents a formidable challenge to healthcare systems and the individuals they serve. Key risk factors for PAD encompass a variety of factors such as age, smoking, diabetes, and hypertension. The convergence of these risk factors underscores the need for heightened awareness and proactive measures to mitigate the disease's progression. By emphasizing the importance of early detection through routine screenings, individuals can take charge of their vascular health and pave the way for timely interventions that can make a lasting impact.
The Current Landscape of PAD in 2023:
With the last act of 2023 about to unfold, the landscape of PAD is marked by a blend of challenges in and advancements of treatments. Recent statistics paint a vivid picture of its global prevalence – affecting millions across various age groups and geographical locations.1 However, this isn't a tale of only despair; medical science has advanced, introducing innovative diagnostic methods and technologies. These developments allow healthcare professionals to detect PAD earlier and with greater precision, enabling tailored treatment approaches for each individual.
What holds promise is the collaboration between healthcare providers and researchers in the ongoing battle against PAD. Collaborative efforts have given rise to approaches that encompass not only medical interventions but also lifestyle modifications, patient education, and support networks. This comprehensive strategy seeks to not only manage the disease but also enhance the overall quality of life for those affected.
Scientific literature is bursting with evidence that highlights the power of group efforts in yielding improved outcomes for patients with PAD. Multidisciplinary care teams, often comprising vascular specialists, cardiologists, physiotherapists, dietitians, and mental health professionals, have demonstrated their efficacy in delivering well-rounded care.2 By harmonizing diverse skill sets and areas of expert knowledge, these teams can address the multifaceted nature of PAD, ranging from medical intricacies to psychological well-being.
The link between healthcare providers and researchers has been instrumental in advancing clinical trials and research endeavors targeting PAD. The fruits of these collaborations are evident in the refinement of existing treatments and the emergence of new therapeutic interventions.2 Furthermore, such partnerships have facilitated the development of tailored treatment plans that align with patients' unique circumstances, enhancing adherence and success.3
Lifestyle modifications are pivotal components of PAD management, and the collaborative approach has amplified their impact. The union of medical insights with behavioral science expertise has resulted in personalized lifestyle recommendations that patients are more likely to adopt and maintain.4 Moreover, patient education initiatives foster informed decision-making, empowering individuals to actively participate in their care journey.
Crucially, shared efforts have not stopped at clinical encounters; they have produced support networks and patient communities. These forums provide a space for individuals affected by PAD to share experiences, garner emotional support, and exchange practical tips for managing the condition.5 Such networks play a pivotal role in alleviating the emotional toll of PAD and fostering a sense of community.
While the strides made by medical professional coordination are remarkable, its impact extends beyond individual patients. Advocacy efforts driven by these partnerships can influence healthcare policies and elevate the prioritization of PAD screening, diagnosis, and treatment on a societal level.6
Behind the scenes, however, lies an economic and societal burden that cannot be ignored. The ripple effects of PAD extend beyond the individual, impacting healthcare systems, workplaces, and families. The strain on resources necessitates a two-pronged approach: equipping healthcare systems to manage the growing caseload of PAD cases and encouraging individuals to adopt preventive measures that can alleviate this burden over time.7 As we navigate this landscape, it becomes clear that our collective efforts hold the potential to shape a future where PAD's impact is minimized and managed effectively.
Emerging Directions in PAD Research and Treatment:
The wide world stage of PAD research and treatment is brightened by promising breakthroughs, ready to transform its narrative. Recent studies have delved deep into the genetic factors that influence susceptibility to PAD. Unraveling the intricate interplay between genes and disease progression not only enhances our understanding but also lays the groundwork for personalized interventions.3
On the frontlines of treatment, a resounding wave of innovations is ushering in a new era, with an intensified spotlight on atherectomy and Chronic Total Occlusion (CTO) crossing procedures. These advanced techniques, including minimally invasive approaches like angioplasty, stenting, and the precision of atherectomy, have undergone metamorphic refinements. These refinements are resulting in enhanced patient outcomes and remarkably shorter recovery times. Alongside these techniques, new medications are being crafted to target the intricate pathways associated with PAD, potentially offering an expansive array of options for healthcare providers.8
One of the most intriguing prospects lies in the realm of personalized treatment. With advances in technology and our growing understanding of individual variability, tailoring treatment plans to a patient's unique genetic makeup, medical history, and lifestyle has moved from the realm of science fiction to scientific reality. This precision-oriented approach not only enhances effectiveness but also minimizes side effects, further underscoring the potential of personalized medicine to transform the PAD treatment landscape.9
As these emerging directions continue to unfold, they cast a beam of hope on those affected by PAD, promising a future where the disease's impact is mitigated and its management is as diverse and dynamic as the individuals it touches.
Preventive Measures for PAD:
Preventing PAD is an act of empowerment that individuals can take to safeguard their vascular health and well-being. A series of impactful lifestyle changes can significantly reduce the risk of developing PAD:
- Say Farewell to Smoking: The decision to quit smoking is one of the most powerful steps you can take. Smoking accelerates artery narrowing, significantly raising the risk of PAD. By kicking this habit, you not only protect your arteries but also those around you from the dangers of secondhand smoke.10
- Step into Movement: Regular exercise isn't just good for your heart – it's also a shield against PAD. Engaging in activities that get your blood pumping promotes healthy blood flow, strengthening your arteries and reducing the risk of blockages.
- A Heart-Healthy Diet: Adopting a balanced diet rich in fruits, vegetables, whole grains, and lean proteins can have a profound impact. These foods support cardiovascular health by reducing inflammation, managing cholesterol levels, and maintaining blood pressure.11
- Tame the Silent Culprits: If you're managing conditions like diabetes or hypertension, staying on top of your treatment plan is paramount. Consistent blood sugar and blood pressure management can prevent further damage to your arteries.
- Weight Matters: Maintaining a healthy weight is a cornerstone of vascular health. Shedding excess pounds can reduce strain on your circulatory system and lower your risk of PAD.
- Routine Health Check-Ups: Regular health check-ups are your armor against PAD. For those with risk factors, routine screenings can catch signs of trouble early on, enabling timely interventions that can make all the difference.
- Empower Yourself: Be proactive about your vascular health. Educate yourself about the risk factors, symptoms, and prevention strategies associated with PAD. By making informed decisions and seeking medical advice when necessary, you take control of your well-being.
Center Stage: Final Impressions
As we stand on the cusp of a new era, the current state of PAD is characterized by promising advancements in diagnostics, treatment, and collaborative efforts among healthcare providers and researchers. Advancements in genetics, pioneering treatments, ongoing clinical trials, and personalized care strategies point us towards a future where PAD management is proactive and customized to individual requirements.
We have journeyed through preventive measures that hold the power to reduce the risk of PAD. From breaking free from the grip of smoking to embracing regular exercise, adopting a heart-healthy diet, and managing underlying conditions, these steps equip us with the tools to safeguard our vascular health. Regular health check-ups and proactive engagement with our own well-being form the bedrock of prevention.
As we draw our exploration to a close, let's not forget the importance of PAD Awareness Month. It's a time to unite, inform, and act. By sharing our knowledge, supporting initiatives, and advocating for change, we can drive a collective effort to elevate PAD awareness to new heights.
Remember, the road to preventing PAD is paved with small yet significant choices. Each positive action you take can be a step toward a future where PAD is not a looming threat but a preventable condition. Your vascular health is in your hands.

Literature Cited
- Yost, M. L. (2023, April). The Current U.S. Prevalence of Peripheral Arterial Disease. Hmpgloballearningnetwork.com. https://www.hmpgloballearningnetwork.com/site/vdm/current-us-prevalence-peripheral-arterial-disease
- Conte, M. S., Bradbury, A. W., Kolh, P., White, J. V., Dick, F., Fitridge, R., ... & Norgren, L. (2019). Global vascular guidelines on the management of chronic limb-threatening ischemia. Journal of Vascular Surgery, 69(6S), 3S-125S.
- Fowkes, F. G., Rudan, D., Rudan, I., Aboyans, V., Denenberg, J. O., McDermott, M. M., ... & Tsilimparis, N. (2013). Comparison of global estimates of prevalence and risk factors for peripheral artery disease in 2000 and 2010: a systematic review and analysis. The Lancet, 382(9901), 1329-1340.
- McDermott, M. M. (2017). Improving functional performance and quality of life in peripheral artery disease. Jama, 317(7), 671-672.
- Rooke, T. W., Hirsch, A. T., Misra, S., Sidawy, A. N., Beckman, J. A., Findeiss, L. K., ... & White, J. C. (2017). 2016 AHA/ACC guideline on the management of patients with lower extremity peripheral artery disease: executive summary. Vascular medicine, 22(3), NP1-NP43.
- Sheets, C. S., & Baker, L. C. (2007). Evaluating the incremental benefits of hospital-academic medical center affiliations. Health Services Research, 42(3pt1), 1103-1121.
- Demsas, F., Joiner, M. M., Telma, K., Flores, A. M., Teklu, S., & Ross, E. G. (2022). Disparities in peripheral artery disease care: A review and call for action. Seminars in vascular surgery, 35(2), 141–154. https://doi.org/10.1053/j.semvascsurg.2022.05.003
- Arabzadeh, A., Faghfuri, E., Razi Soofiyani, S., Dalir Abdolahinia, E., Siapush, S., Nejati-Koshki, K., Shahrami, B., Asghariazar, V., & Pahlavan, Y. (2023). Current and Novel Emerging Medical Therapies for Peripheral Artery Disease: A Literature Review. Advanced pharmaceutical bulletin, 13(2), 259–268. https://doi.org/10.34172/apb.2023.025
- Salybekov, A. A., Wolfien, M., Kobayashi, S., Steinhoff, G., & Asahara, T. (2021). Personalized Cell Therapy for Patients with Peripheral Arterial Diseases in the Context of Genetic Alterations: Artificial Intelligence-Based Responder and Non-Responder Prediction. Cells, 10(12), 3266. MDPI AG. Retrieved from http://dx.doi.org/10.3390/cells10123266
- Wang, W., Zhao, T., Geng, K., Yuan, G., Chen, Y., & Xu, Y. (2021). Smoking and the Pathophysiology of Peripheral Artery Disease. Frontiers in cardiovascular medicine, 8, 704106. https://doi.org/10.3389/fcvm.2021.704106
- Nosova, E. V., Conte, M. S., & Grenon, S. M. (2015). Advancing beyond the "heart-healthy diet" for peripheral arterial disease. Journal of vascular surgery, 61(1), 265–274. https://doi.org/10.1016/j.jvs.2014.10.022