Topics: Peripheral Artery Disease, Atherectomy, Diabetes, Leg pain, Amputation, PAD Diagnosis, PAD
In 2007, a global initiative was set in motion by the American College of Sports Medicine, endorsed by both the American Medical Association and the Office of the Surgeon General. This initiative aimed to rally physicians, healthcare professionals, providers, and educators in advocating for exercise to prevent, mitigate, manage, or treat diseases that impact individuals' health and overall quality of life.

One of the most significant diseases this was aimed at is Peripheral Artery Disease (PAD). PAD is a chronic condition primarily affecting the arteries that supply blood to the limbs, especially the legs. PAD results from atherosclerosis, a gradual buildup of fatty plaques on artery walls. These plaques narrow and stiffen the arteries, reducing blood flow and causing symptoms like claudication, leg pain during activities. PAD typically progresses silently, making early detection crucial. Left untreated, it can lead to severe complications, including non-healing ulcers, tissue damage, and an increased risk of heart attacks and strokes. Exercise Therapy (ET) is a key part of PAD management, enhancing blood circulation, alleviating symptoms, and improving cardiovascular health.
The Clinical Advantages of Exercise Therapy (ET) for PAD
The clinical advantages of ET for individuals with PAD came into the spotlight in 1966, with a study conducted in Denmark.1 In this study, 14 patients were randomly assigned to either ET or a placebo group. Notably, the 7 patients who underwent ET demonstrated an increase in walking distance, both before the onset of claudication and in total walking distance. Reinforcing the significance of ET, the 2016 ACC/AHA Guidelines provide a Class 1A (the highest) recommendation for supervised exercise programs for patients grappling with claudication.2
Personalized Exercise Programs for PAD
The Mayo Clinic Proceedings recently conducted an extensive examination of the latest information regarding PAD and ET, encompassing its risk factors, treatment choices, and results. When it comes to initiating a structured exercise program for individuals dealing with PAD, the first step involves a comprehensive assessment of various patient factors.
This assessment considers elements like the individual's current activity level, age, gender, and any potential challenges that may affect their ability to engage in physical activity. Following this, exercise testing is conducted to evaluate aspects related to the body's response to exercise, including parameters like hemodynamics (how blood flow responds), signs and symptoms experienced during exercise, changes in the ST segment of the electrocardiogram (The ST segment is a part of the heart's electrical pattern shown on an ECG, or heart monitor), and overall exercise capacity.
This thorough evaluation helps to categorize patients into different risk levels which guides decisions about the level of supervision and monitoring needed during the exercise program. Finally, based on all these factors, a personalized exercise plan is developed to ensure the most effective and safe approach for each individual.
Exercise Types for PAD
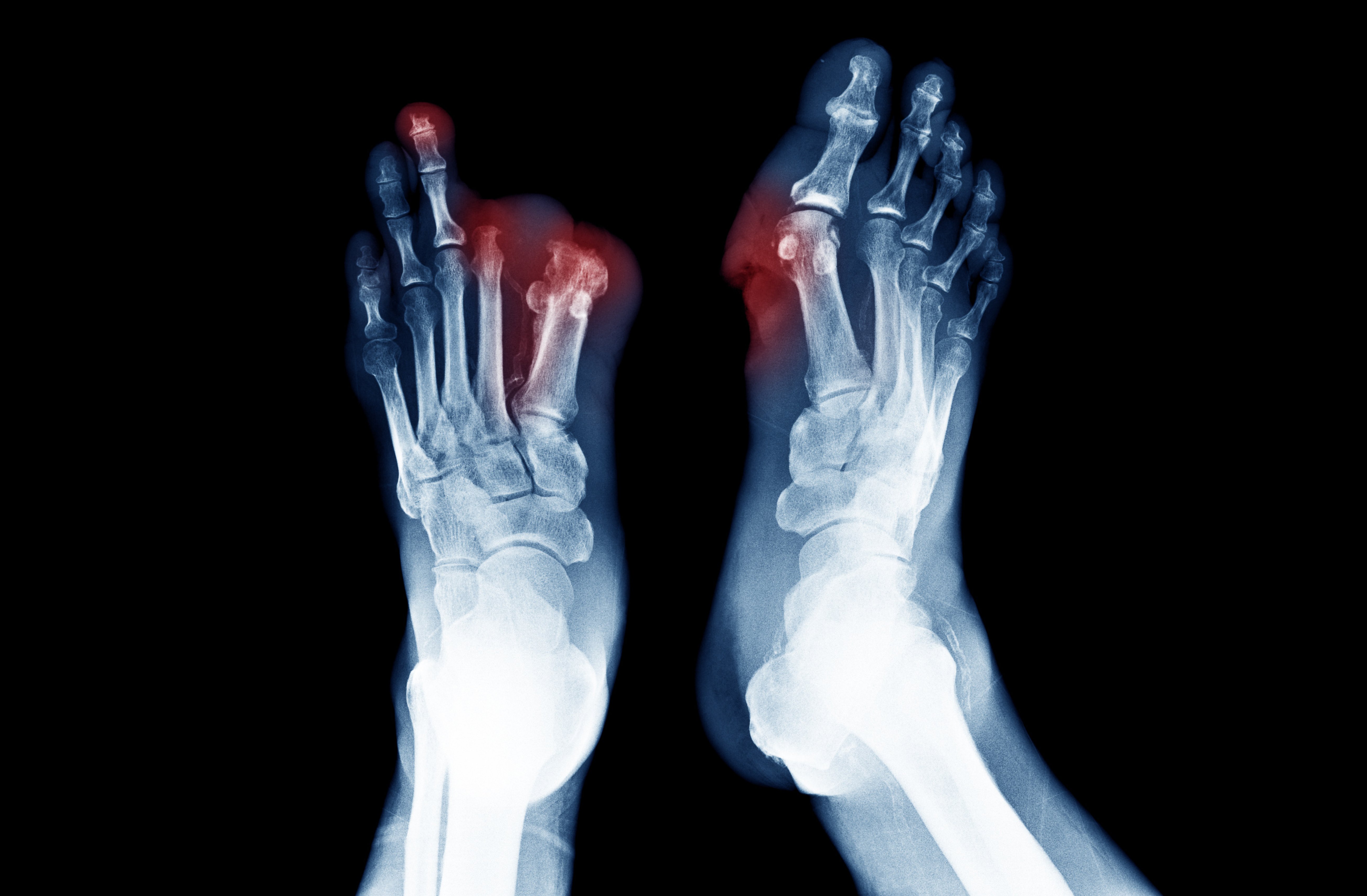
Regarding the choice of exercise for PAD, treadmill walking stands out as the most strongly supported option, and it's currently the preferred approach. Alternatives like cycling or arm-cranking (using the arms to pedal or crank a machine that resembles a stationary bicycle) have also shown benefits, particularly in terms of maximizing walking time. 4 When it comes to the type of exercise, aerobic training is generally favored over resistance training. Additionally, there are other exercise methods to consider, such as total body recumbent stepping training, descending stair walking, and non-weight-bearing exercises. These alternatives may offer similar effectiveness to treadmill walking and can be especially beneficial for individuals facing obstacles to treadmill use, such as those with diabetic foot ulcers.
Recommended Exercise Duration and Frequency
The current recommendations from the American College of Cardiology (ACC) and the American Heart Association (AHA) advise individuals to engage in exercise sessions for PAD management. It's recommended to aim for a minimum of three exercise sessions per week.These sessions should ideally last between 30 to 60 minutes, with more recent data suggesting that the most substantial improvement tends to occur around the 45-minute mark.5 It's worth noting that there isn't a standardized duration for ET, and positive effects have been observed in as little as two months.
Physiological Mechanisms Behind ET's Benefits for PAD
Several physiological mechanisms contribute to the positive outcomes of ET, including enhancements in skeletal muscle oxidative metabolism, improved formation of arterial collateral blood vessels, better functioning of the endothelium (the inner lining of blood vessels), increased lipid metabolism, and reduced levels of inflammation in the body.
- Improved Skeletal Muscle Oxidative Metabolism: Acylcarnitine is a substance in our body that helps with two important things: making energy in our cells and creating essential molecules. When there's too much acylcarnitine, it can cause problems like muscle stress and difficulty using insulin. People with a condition called PAD often have too much acylcarnitine in their blood because their blood flow is reduced. This extra acylcarnitine makes it harder for them to move well, but when their muscles get better at using oxygen and fuel, the extra acylcarnitine decreases. This helps people with PAD feel and move better.3
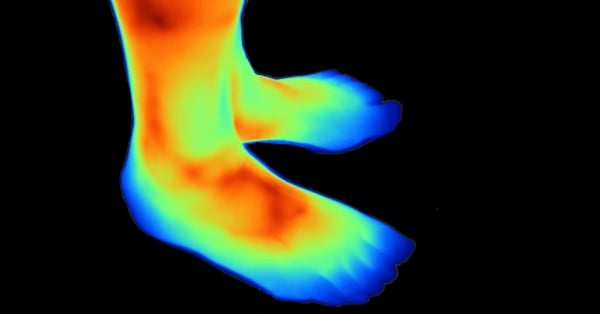
- Enhanced Arterial Collateralization: Claudication pain arises when the muscles don't receive enough oxygen and nutrients due to limited blood flow during physical activity. Exercise has been suggested to potentially improve this situation in people with PAD by enhancing the circulation of blood through collateral vessels in the legs. Some animal studies, have shown promising results, demonstrating increased collateral blood flow in exercise-trained animals.3
- Improved Endothelial Function: Endothelial dysfunction is when the inner lining of blood vessels doesn't work properly, which can cause problems with blood flow and vessel health. In the case of PAD, which is a condition where blood flow to the legs is reduced, endothelial dysfunction can both contribute to its development and be worsened by it. Studies have shown that exercise can be beneficial for the inner lining of blood vessels. For example, one study involving 111 PAD patients in 2009 found that people who were more physically active had blood vessels in their arms that could expand better when needed.6
- Increased Lipid Metabolism: Both aerobic exercise and resistance training, when performed at moderate intensity, have shown the ability to notably increase levels of high-density lipoprotein cholesterol (HDL-C), which is often referred to as "good" cholesterol. Additionally, higher intensity exercise goes a step further by contributing to reductions in levels of low-density lipoprotein cholesterol (LDL-C) and triglycerides within the general population. This is significant because LDL-C and triglycerides are considered "bad" forms of cholesterol, and reducing them can benefit overall cardiovascular health.7
In simpler terms, both aerobic and resistance exercises, especially when performed moderately or with higher intensity, can improve cholesterol levels and help control blood pressure. This can have a positive impact on reducing the risk factors for PAD and promoting overall cardiovascular health. - Reduced Inflammatory Activation: Numerous inflammatory molecules have been identified as contributors to the development of PAD. These include substances like C-reactive protein, interleukin-6, soluble intercellular adhesion molecule-1, D-dimer, and homocysteine. Notably, these molecules not only have links to the initial onset of PAD but also serve as predictive indicators for disease progression, severity, and the likelihood of developing complications.8
Exercise plays a significant therapeutic role in individuals with PAD by addressing this inflammatory activation. In essence, exercise helps to decrease or suppress the inflammatory response, potentially mitigating the severity of the disease.
Outcomes: ET's Impact on Walking Ability
The positive effects of ET on walking ability have been examined across various studies. For instance, in the PROPEL trial, individuals who participated in exercise alone experienced a significant improvement in their 6-minute walk distance (a commonly used measure of walking ability), covering an additional distance of 33.6 meters. In a separate randomized controlled trial, the ET group demonstrated an even more substantial increase of 35.9 meters in their 6-minute walk distance. It's worth noting that this particular study included all patients with an ankle-brachial index (ABI) below 0.95, regardless of whether they had claudication symptoms or not.9
In the CLEVER trial, which compared stenting to ET, it was found that ET improved peak walking time, despite the fact that stenting led to a greater improvement in ABI (a measure of blood flow) compared to ET. Another study showed that ET was effective in enhancing walking distance, both in individuals experiencing initial claudication (mild leg pain during exercise) and those with more severe claudication, without necessarily improving the ABI.10
Additionally, the EXITPAD trial highlighted the significance of supervised ET in improving both walking distance and quality of life when compared to unsupervised ET. A systematic review that examined various modes and intensities of ET revealed consistent positive outcomes, indicating that most forms of exercise resulted in significant improvements in walking capability.11
Clearly, numerous studies have demonstrated that ET can substantially enhance a person's ability to walk, regardless of the severity of their PAD symptoms or the specific type of exercise program used.
ET's Influence on Mortality Risk in PAD
Individuals with PAD who demonstrate higher baseline functional performance, as assessed by tests like the 6-minute walk distance (6MWD) and a 4-meter walk speed, tend to have a lower risk of mortality compared to those with lower baseline functional performance. Furthermore, a decrease in the total walking distance over time has been identified as a potential indicator of higher mortality risk.
While there are no randomized controlled trials specifically assessing mortality in PAD patients undergoing ET versus those without such therapy, retrospective data has shed light on the potential survival benefits of ET for PAD. For instance, in a significant retrospective study focusing on patients with claudication, it was discovered that patients who received primary ET had lower mortality rates and underwent fewer revascularization procedures compared to those who opted for endovascular or surgical revascularization.12 It's important to note that this study excluded patients with Critical Limb Ischemia (CLI), and current evidence does not support delaying revascularization for CLI. Instead, this data highlights the potential of ET as a primary treatment for PAD without CLI.
Challenges in Promoting ET for PAD
Despite the notable strides in PAD treatment, the utilization of ET, considered a primary treatment, remains surprisingly low. Intriguingly, the data concerning ET for PAD lags behind that of cardiac rehabilitation for conditions like Coronary Artery Disease (CAD) and heart failure, despite the considerable health risks associated with PAD. It's imperative to advocate for the establishment of Structured Exercise Therapy (SET) programs to enhance nationwide outcomes for PAD patients. The call to action extends to healthcare professionals and public health leaders who should actively promote physical activity among patients and the wider population to harness the associated health benefits and contribute to global health improvement.
Harnessing the Potential of Exercise Therapy for PAD
PAD is an increasingly prevalent and largely preventable condition. Uncontrolled PAD can exact a heavy toll, causing a decline in quality of life, disability, amputation, and even fatality. Fortunately, ET emerges as a highly effective initial treatment for PAD, delivering clear benefits while posing minimal risks; However, its adoption remains suboptimal, and the need for further research in this realm persists.
The body of evidence firmly substantiates the pivotal role of ET in both preventing and managing PAD, leading to enhancements in symptom management, walking capability, overall well-being, and a reduction in major cardiovascular events among affected individuals. Moving forward, the evolution of ET for PAD should encompass the creation of guidelines tailored to individual patient requirements, particularly catering to those unable to partake in standard treadmill exercises for various reasons. The critical aspect of identifying and addressing barriers to integrating SET into routine PAD care at individual healthcare facilities also warrants focused efforts.
While ET holds substantial potential as a leading treatment for PAD, it is imperative to heighten awareness, tailor programs to individual needs, and surmount obstacles to ensure that a broader spectrum of patients can benefit from this proven therapeutic approach.

Take Action:
If you or a loved one is suffering from the possibility of amputation, take action today. Find a doctor who performs Lumivascular procedures in your area. Lumivascular atherectomy allows your doctor to see inside of your arteries and safely restore blood flow in the affected artery. Improve blood flow in your arteries, find a Lumivascular doctor today.
Literature Cited
- Larsen, O. A., & Lassen, N. A. (1966). Effect of daily muscular exercise in patients with intermittent claudication. Lancet (London, England), 2(7473), 1093–1096.
- Gerhard-Herman, M. D., Gornik, H. L., Barrett, C., Barshes, N. R., Corriere, M. A., Drachman, D. E., Fleisher, L. A., Fowkes, F. G., Hamburg, N. M., Kinlay, S., Lookstein, R., Misra, S., Mureebe, L., Olin, J. W., Patel, R. A., Regensteiner, J. G., Schanzer, A., Shishehbor, M. H., Stewart, K. J., Treat-Jacobson, D., … Walsh, M. E. (2017). 2016 AHA/ACC Guideline on the Management of Patients With Lower Extremity Peripheral Artery Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation, 135(12), e726–e779.
- Hallak, A. O., Hallak, F. Z., Hallak, Y. O., Hallak, O. O., Hayson, A. W., Tanami, S. A., Bennett, W. L., & Lavie, C. J. (2023). Exercise Therapy in the Management of Peripheral Arterial Disease. Mayo Clinic proceedings. Innovations, quality & outcomes, 7(5), 476–489.
- Norgren, L., Hiatt, W. R., Dormandy, J. A., Nehler, M. R., Harris, K. A., Fowkes, F. G., & TASC II Working Group (2007). Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II). Journal of vascular surgery, 45 Suppl S, S5–S67.
- Top of Form Bulmer, A. C., & Coombes, J. S. (2004). Optimising exercise training in peripheral arterial disease. Sports medicine (Auckland, N.Z.), 34(14), 983–1003.
- Payvandi L., Dyer A., McPherson D., et al. Physical activity during daily life and brachial artery flow-mediated dilation in peripheral arterial disease. Vasc Med. 2009;14(3):193–201.
- Hamburg N.M., Balady G.J. Exercise rehabilitation in peripheral artery disease: functional impact and mechanisms of benefits. Circulation. 2011;123(1):87–97.
- Li J.J., Fang C.H. C-reactive protein is not only an inflammatory marker but also a direct cause of cardiovascular diseases. Med Hypotheses. 2004;62(4):499–506.
- McDermott M.M., Ades P., Guralnik J.M., et al. Treadmill exercise and resistance training in patients with peripheral arterial disease with and without intermittent claudication: a randomized controlled trial. JAMA. 2009;301(2):165–174.
- Murphy T.P., Cutlip D.E., Regensteiner J.G., et al. Supervised exercise versus primary stenting for claudication resulting from aortoiliac peripheral artery disease: six-month outcomes from the claudication: exercise versus endoluminal revascularization (CLEVER) study. Circulation. 2012;125(1):130–139.
- Nicolaï S.P., Teijink J.A., Prins M.H. Exercise Therapy in Peripheral Arterial Disease Study Group. Multicenter randomized clinical trial of supervised exercise therapy with or without feedback versus walking advice for intermittent claudication. J Vasc Surg. 2010;52(2):348–355.
- Jansen S.C.P., van Nistelrooij L.P.J., Scheltinga M.R.M., Rouwet E.V., Teijink J.A.W., Vahl A.C. Successful implementation of the exercise first approach for intermittent claudication in the Netherlands is associated with few lower limb revascularisations. Eur J Vasc Endovasc Surg. 2020;60(6):881–887.