Topics: Peripheral Artery Disease, Lumivascular, Diabetes, Gangrene, Amputation
Limb loss is a serious problem affecting nearly 2 million people in the United States alone. And among those living with limb loss, 54% of them are because of diabetes and Peripheral Artery Disease (PAD).1
What is Peripheral Artery Disease?
Now that we know that Peripheral Artery Disease (PAD) is linked to diabetes and amputation, it is important to understand what the disease is and what the symptoms include.
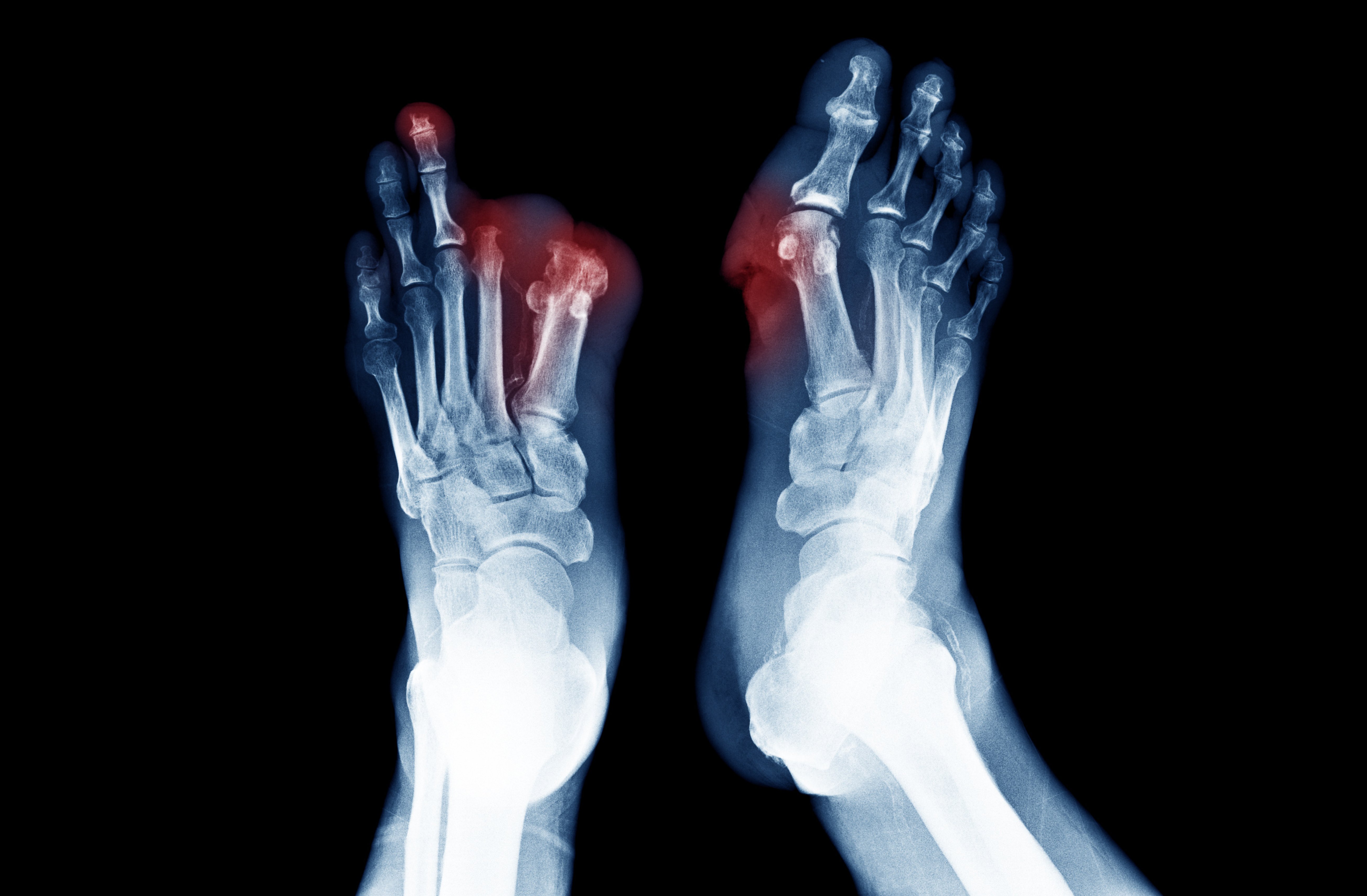
PAD is a disease where patient experience atherosclerosis in the arteries of their legs and feet. There are numerous symptoms that patients with PAD will have while others will experience just a few. Interestingly, over 50% of all patients diagnosed with PAD have no symptoms at all.2 Just some of the symptoms of Peripheral Artery Disease includes severe cramping in the leg after walking or exercising due to the intermittent claudication in the arteries. This leg pain will typically dissipate after rest.
Another symptom of Peripheral Artery disease is gangrene that can develop in the areas of the feet where the blood supply is lost because of the obstruction and blockage in the arteries. Patients experiencing symptoms of gangrene will find that this dead tissue or gangrene on their toes. Patients who are experiencing symptoms of PAD like gangrene or dead tissue should seek medical treatment immediately as gangrene can lead to amputation of a limb if left untreated.
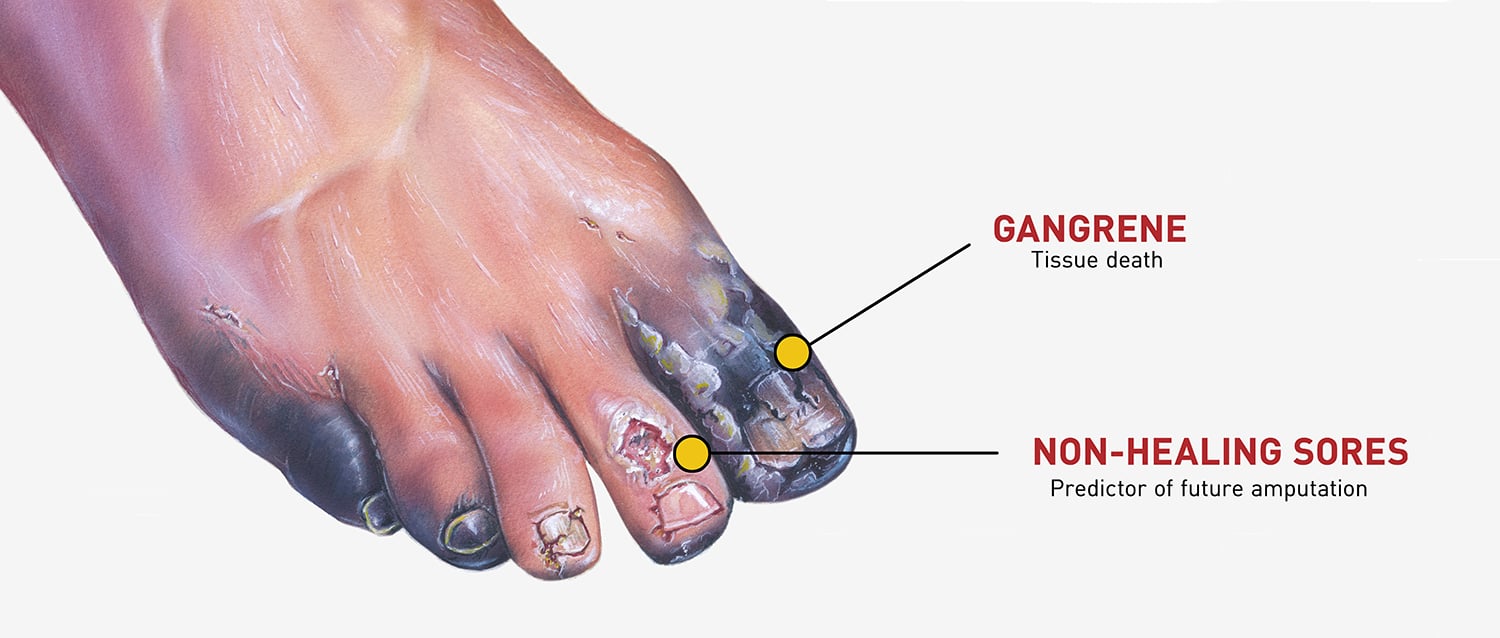 One of the symptoms of PAD that leads to amputation is lower extremity sores that will not heal. These chronic wounds on the legs and feet cannot heal themselves because there is not enough healthy blood flow to the lower extremities. Neglected ulcers and wounds on the legs of patients with Peripheral Artery Disease, can quickly become a very serious problem that can lead to amputation.
One of the symptoms of PAD that leads to amputation is lower extremity sores that will not heal. These chronic wounds on the legs and feet cannot heal themselves because there is not enough healthy blood flow to the lower extremities. Neglected ulcers and wounds on the legs of patients with Peripheral Artery Disease, can quickly become a very serious problem that can lead to amputation.
Connection Between Diabetes and Amputation
 Amputation due to diabetes is more common than the average person may believe. But why do diabetics lose limbs? According to the World Health Organization, lower-extremity amputations are 10 times more likely in patients with diabetes than in people who do not have diabetes.3
Amputation due to diabetes is more common than the average person may believe. But why do diabetics lose limbs? According to the World Health Organization, lower-extremity amputations are 10 times more likely in patients with diabetes than in people who do not have diabetes.3
With nearly 60% of amputations being due to common complications of diabetes and peripheral artery disease,1 it is important to address the connection between the two so that future patients can seek help and save their limb before it is too late.
The problem is that patients with diabetes suffer from peripheral neuropathy which essentially is a loss of sensation in their feet and legs that they are not alerted to the potential dangers of walking on their sore and open ulcers on their legs and feet that they get from Peripheral Artery Disease. Some patients with peripheral neuropathy may even step on a nail without being able to feel the pain at all. Therefore, when the effects of poor circulation and open wounds of PAD are combined with the peripheral neuropathy of diabetes, it can really put a patients’ legs and feet at risk for amputation.
When the symptoms of peripheral neuropathy are combined with the effects of Peripheral Artery Disease, it explains why so many diabetes patients require amputation, they simply cannot feel the open sores on their legs and feet until are at a high risk of amputation and are nearing a point of no return. However, with proper treatment, education and follow-up care, there is no reason why many of these high-risk patients cannot be healed.
The Cost of Amputation
Every single year over 185,000 amputations occur in the United States.4 However, there are many serious negative side effects that come with limb amputation. For example, lower-extremity amputations in patients with diabetes generally comes with yearly costs between $30,000 and $60,000 and lifetime costs of half a million dollars.3 Although there are occasions where amputations are medically necessary, if the limb loss can be prevented it is the most cost effective for the patient.
Additionally, almost half of the individuals who have an amputation due to vascular disease will pass away within five years of the amputation. This is statistic is even higher than the five-year mortality rates for breast cancer, colon cancer, and prostate cancer.5
Patients with diabetes also risk having their second leg amputated. Up to 55% of patients who have had one leg amputated will need an amputation of their second leg within 2‐3 years. For many people, having both legs amputated will negatively impact their way of life.6
Reasons to Prevent Amputation
The chairman of the International Diabetes Federation, Dr. Karel Bakker believes that up to 85% of amputation procedures would be rendered unnecessary if there were more effective foot care and patient strategies implemented.7 Nearly 90% of the non-traumatic foot and leg amputation in the United States come from the development of infected foot ulcers that cannot heal without proper treatment.8 Because there is not enough healthy blood flow going to the feet, these ulcers cannot heal and they quickly spread and destroy the surrounding foot tissue.
In addition, a recent study found that attempting to restore healthy blow flow may be a better treatment than amputation for patients suffering from critical lower limb circulation problems. Limb amputation is associated with numerous poor outcomes like loss of independence, shortened lifespan and depression. The issue is that many patients are told that amputation is their only option.
"If you or a family member or a friend or a neighbor has poor circulation, and someone has told them that they need an amputation, please seek a second opinion."
This is why it is so crucial that patients always seek a second opinion before committing to amputation. Many patients are never informed that there is an alternative to amputation and that amputation is not the only solution to their problems. A second opinion could be the difference between life and limb for thousands of patients with diabetes and Peripheral Artery Disease each year.
Lumivascular Procedure to Restore Blood Flow
As previously mentioned, taking preventative methods can be a crucial method for preventing amputation and limb loss. If you have diabetes and are diagnosed with PAD, talking to a physician to see if you are a good candidate for a Lumivascular atherectomy is a great proactive measure. Waiting to get help and treatment will only cause your poor circulation and gangrene to worsen.
Lumivascular atherectomy is a technological advancement that uses imaging on the end of a catheter. This camera-like imaging system allows a physician to see inside the patients’ artery in real time while they move through the blockage.
Throughout the entire procedure, your physician will be able to clearly see inside the obstructed artery and see the difference between your healthy and diseased tissue. Additionally, your physician will then be able to remove as much plaque as is needed. After the Lumivascular procedure, the hope is that you will be able to improve the circulation of your foot and leg because of the restoration of a health blood flow through your artery.
Patients experiencing any of these symptoms of Peripheral Artery Disease (PAD) should go to a doctor and get an official diagnosis so they can prevent limb amputation. If you have Peripheral Artery Disease, a Lumivascular atherectomy may be the best treatment option for you. If you are diagnosed with peripheral artery disease and want to improve the blood flow to your arteries in your lower limbs, ask your doctor if the Lumivascular atherectomy could work for you. Click here to find a Lumivascular atherectomy doctor nearest you.
Take Action:
- Patient Story: Watch how Chuck Lyon prevented getting an amputation
- Learn more about Lumivascular atherectomy
- Find a Lumivascular doctor in your area
Related Articles:
- 14 Fast Facts About Diabetic Foot Disease and Peripheral Artery Disease
- Diabetes and Peripheral Artery Disease
If you have found this article helpful, please don’t forget to share!
References:
- Ziegler‐Graham, et al. Estimating the Prevalence of Limb Loss in the United States: 2005 to 2050. Archives of Physical Medicine and Rehabilitation 2008;89(3):422‐9.
- McDermott, M. Lower Extremity Manifestations of Peripheral Artery Disease. Circ Res 2015
- Hoffstad, et al. Diabetes, Lower-Extremity Amputation, and Death. Diabetes Care 2015 Oct; 38(10): 1852-1857.
- Owings M, Kozak LJ, National Center for Health S. Ambulatory and Inpatient Procedures in the United States, 1996. Hyattsville, Md.: U.S. Dept. of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics; 1998.
- Robbins, et al. Mortality Rates and Diabetic Foot Ulcers. Journal of the American Podiatric Medical Association2008 November 1, 2008;98(6):489‐93.
- Pandian, et al. Rehabilitation of the Patient with Peripheral Vascular Disease and Diabetic Foot Problems. In: DeLisa JA, Gans BM, editors. Philadelphia: Lippincott‐Raven; 1998.
- Bakker, et al. Step by Step, improving diabetic foot care in the developing world. Practical Diabetes Int. 2006; 23(8): 365–369
- Pecoraro, et al. Pathways to diabetic limb amputation: basis for prevention. Diabetes Care 1990;13:513-21.