Topics: Peripheral Artery Disease, Critical Limb Ischemia, Atherosclerosis, Lumivascular, Gangrene, PAD Symptoms, intermittent claudication, Poor Circulation
Your body’s cardiovascular system moves the life-supporting blood throughout your body. It allows your heart to beat, your body to move, and your brain to process. When this natural blood flow isn’t working properly, it can lead to symptoms that initially appear in the feet and legs.
These symptoms are driven by Peripheral Artery Disease or PAD.
Intermittent claudication refers to the pain and cramping in the legs that occurs with exercise and goes away after rest. The most common location of intermittent claudication is the calf muscle of the leg, leading to calf or leg pain while walking. The pain in the calf muscle occurs only during exercise such as walking, and the pain steadily increases with continued walking until the patient has to stop due to intolerable pain. Then the pain quickly goes away during rest. Peripheral artery disease related intermittent claudication can affect one or both legs.
Rest pain in the legs happens when not enough blood and oxygen get to the legs even while resting and the pain may wake you up while sleeping. Rest pain represents a more serious form of the condition called critical limb ischemia.
Patients with PAD have a broad range of symptoms other than classic intermittent claudication.1 Other symptoms and signs of peripheral artery disease include:
- Numbness of the legs or feet
- Weakness and atrophy (diminished size and strength) of the calf muscle
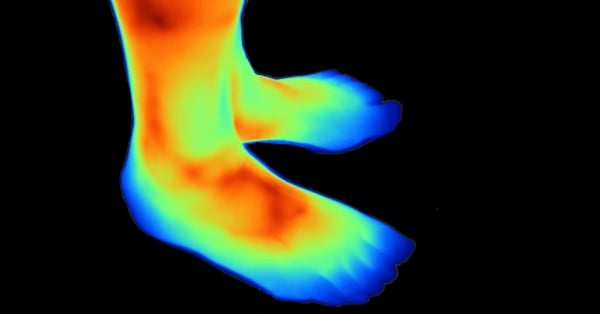
- A feeling of coldness in the legs or feet
- Changes in color of the feet; feet turn pale when they are elevated, and turn dusky red in dependent position
- Hair loss over the top of the feet and thickening of the toenails
- Poor wound healing in the legs or feet
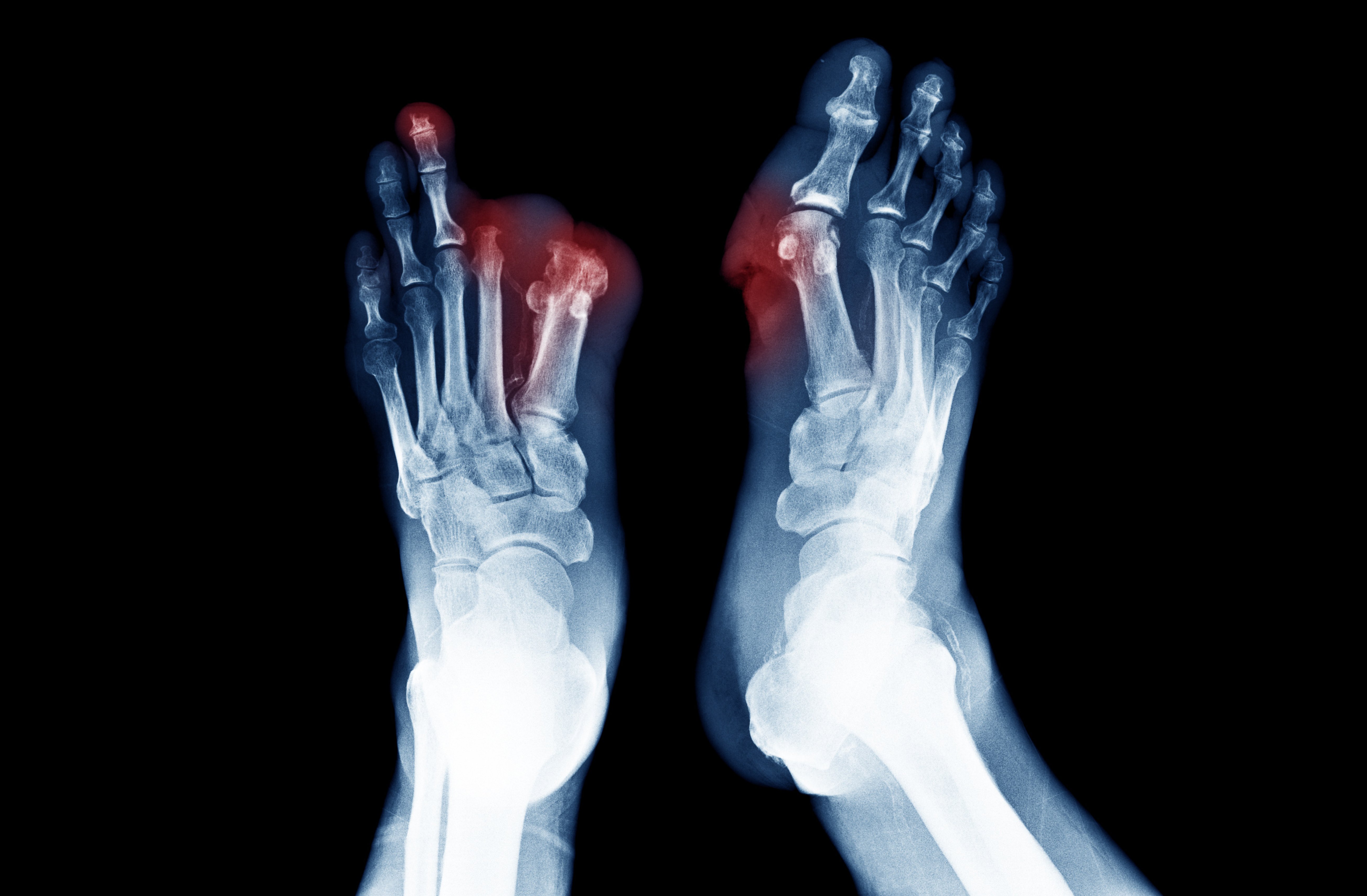
- Painful ulcers and/or gangrene in areas of the feet where blood supply is lost; typically in the toes
Secondary Signs and Symptoms of PAD include:
Foot Ulcers
Diabetic foot ulcers are a common and feared complication of diabetes. Recent studies suggest that the lifetime risk of developing a foot ulcer in diabetic patients may be as high as 25%.2 Foot ulceration requires long and intensive treatment and has important effects on quality of life of both patients and care-givers.3
Non-Healing Wounds
Non-healing wounds are chronic sores on the toes, feet, or legs that aren’t healing well.4,5 PAD can reduce blood flow to the extremities and can make it difficult for the body to heal itself. Critical limb ischemia is also associated with wounds that heal slowly. This severe form of peripheral artery disease can result in ulcers below the ankle and non-healing wounds between toes. Up to 2 million people in the United States suffer from leg ulcers or non-healing wounds.6
Foot Infections
Non-healing wounds on the feet can become infected. There are many painful consequences associated with untreated foot infections. One of those consequences is tissue death, which is commonly known as gangrene.
Tissue Loss
Prevention of wounds through patient education, foot examination, and quick recognition of foot infection are important methods to minimize tissue loss among patients with PAD.
Skin Color Changes
If there isn’t enough arterial blood reaching the body's tissues, the skin may appear pale or blue. Also, if blood is leaking from capillaries, these areas may appear purple.
A Feeling of Coldness in the Legs or Feet
Poor circulation due to atherosclerosis can make it difficult for enough warm blood to get to your feet regularly, which means that your feet will be cooler than the rest of your body.
Erectile dysfunction
While erectile dysfunction has many causes, one of the most common causes is peripheral arterial disease (PAD). Erectile dysfunction (ED) signals underlying cardiovascular problems like atherosclerosis.7 In addition, men with erectile dysfunction were found to have significantly higher prevalence of PAD than men without erectile dysfunction.
Depression
Symptoms of depression are commonly associated with PAD. These peripheral artierial disease patients are often restricted in physical function and may experience depression.1
Because patients with PAD have a high prevalence of comorbid disease and exertional leg symptoms, the relationship between depressive symptoms and physical symptoms associated with walking impairment might be different in patients with PAD and patients without PAD.
Gangrene
Gangrene in your toes occurs when body tissue dies. When atherosclerosis causes total loss of circulation to the legs and feet, gangrene can develop and result in the loss of a limb. This limb-threatening manifestations of “end game” PAD is known as Critical Limb Ischemia (CLI).
Asymptomatic Peripheral Artery Disease
The term asymptomatic means showing no symptoms. When that term is used with peripheral artery disease, it describes a condition that is present, but the person does not show any outward signs or symptoms of the peripheral artery disease. About 40% of all people diagnosed with PAD have no symptoms.8
In a study, more than half of the inactive people that say they don’t have any exertional leg pain developed leg pain during the 6-minute walk. This suggests that some participants were simply walking less to avoid leg pain symptoms. Possibly some of them had previously experienced exertional leg symptoms and limited their activity to avoid the pain. This could explain why 20% of persons with PAD reported no exertional leg pain symptoms, despite prior referral to the vascular laboratory.1
The nature of leg symptoms predict the degree of functional decline after two years.9. Participants with peripheral artery disease having leg pain after exercise and rest experienced greater declines in walking endurance and walking speed than people without PAD.
In previous studies, most patients with intermittent claudication reported improvement or stabilization in leg symptoms over 5 years of follow-up. This implies that there is a benign natural history of lower-extremity functioning in those with PAD. However, stabilization or improvement in claudication symptoms does not necessarily mean that there is stabilization or improvement in lower-extremity performance. Claudication symptoms may lessen because of lower levels of physical activity. Our data suggests that stabilization of claudication symptoms over time may be more related to declining functional performance than to lack of PAD progression.9
Decreased Physical Function
Patients with peripheral arterial disease have reduced functioning when compared to individuals without PAD. 1,10,11 The greater severity of PAD symptoms, the greater impairment of lower extremity functioning.10,11
Reduced lower extremity functioning is an important predictor of future disability, mobility loss, and nursing home placement.12,13
Treatment Options
When you develop poor circulation, the plaque is the problem. Similar to a clogged pipe under your house, you need someone to pull out the debris backing up your pipes. A Lumivascular atherectomy does just that. Through a minimally invasive procedure, your physician can reach your blockage and remove the plaque. One huge advantage to a Lumivascular atherectomy is that your physician can see – yes, see inside – your vessel. This helps them to visualize what needs to be removed and avoid injuring the healthy lining of your vessels that may lead to developing blockage again.
If you are looking to reverse the cycle of symptoms due to poor blood flow, please click here to find a Lumivascular atherectomy physician in your area.
Take Action:
- Learn more about Lumivascular atherectomy
- Find a Lumivascular doctor in your area
If you have found this article helpful, please don’t forget to share!
References:
- McDermott, et al. Leg Symptoms in Peripheral Arterial Disease. Associated Clinical Characteristics and Functional Impairment. JAMA. 2001;286(13):1599-1606
- Singh, et al. Preventing foot ulcers in patients with diabetes. JAMA 2005; 293:217–228
- Nabuurs-Franssen, et al. Health-related quality of life of diabetic foot ulcer patients and their caregivers. Diabetologia 2005; 48:1906–1910
- Iqbal, et al. Management of Chronic Non-healing Wounds by Hirudotherapy. World J Plast Surg. 2017 Jan; 6(1): 9–17.
- Hess, T. Checklist for Factors Affecting Wound Healing. Advances in Skin & Wound Care: April 2011
- Margolis, et al. Venous leg ulcer: incidence and prevalence in the elderly. J Am Acad Dermatol 2002;46(3):381-6.
- Polonsky, et al. The association between erectile dysfunction and peripheral arterial disease as determined by screening ankle-brachial index testing. 2009;207(2):440-4.
- Hirsch, et al. Peripheral arterial disease detection, awareness, and treatment in primary care. JAMA. 2001;286(11):1317-1324.
- McDermott, et al.Functional Decline in Peripheral Arterial Disease: Associations With the Ankle Brachial Index and Leg Symptoms. 2004;292(4):453-461.
- McDermott, et al. Asymptomatic peripheral arterial disease is independently associated with impaired lower extremity functioning: the Women’s Health and Aging Study. Circulation. 2000;101:1007–12.
- McDermott, et al. Lower extremity performance is associated with daily life physical activity in individuals with and without peripheral arterial disease. J Am Geriatr Soc. 2002 Feb;50(2):247-55.
- Guralnik, et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol 49:M85–M94, 1994
- Guralnik, et al. Lower extremity function in persons over 70 years as a predictor of subsequent disability. N Engl J Med. 1995; 332:556–561,