Topics: Peripheral Artery Disease, Atherectomy, Leg pain, Women, Gender
A Scientific Statement on Women’s Higher Risk For Developing Peripheral Artery Disease.
As new information is coming to light about the prevalence of peripheral artery disease (PAD), the question remains who is susceptible to PAD? PAD is an increasing worldwide burden with its prevalence now larger than and outpacing diseases like cancer, stroke, and Alzheimer’s. Approximately 10% of the U.S. population has PAD, equating to almost 33 million citizens1. “Lower extremity PAD is known to be associated with equal morbidity and mortality and comparable (or higher) health economic costs as coronary heart disease (CHD) and ischemic stroke.”2 Conventional data has shown that women “suffer the consequences of PAD at rates at least as high as those observed in men”2 but a scientific statement from the American Heart Association illustrates a more complicated story.
.jpeg)
This scientific statement, published by the American Heart Association and endorsed by the Vascular Disease Foundation and its Peripheral Artery Disease Coalition, notes that women are more prone to develop PAD as they age, have higher morbidity and mortality rates, are more likely to not have typical PAD symptoms, and less likely to receive care for their PAD.

Figure 1: Estimated Gender-specific burden of peripheral artery disease (PAD) by age group.
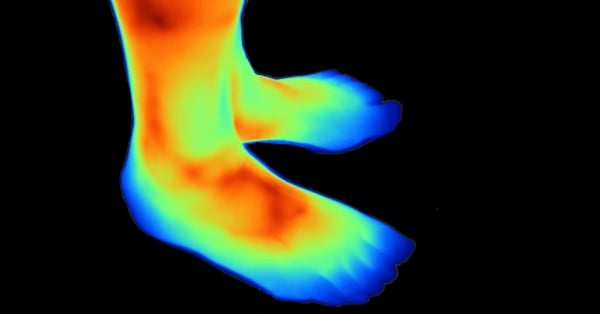
The analysis demonstrates that PAD increases with age for both men and women especially when factoring in environmental factors like nutrition, exercise, and lifestyle. “Using US census data from 2010, the burden of PAD was calculated and showed that there were more women than men with PAD among US adults ≥ 40 years of age”2 PAD can affect women more severely than men due to their smaller vasculature, which can cause the disease to act rapidly and limit their mobility or lead to a decline in their quality of life. One explanation as to why women are not screened or treated often enough may relate to the fact that “asymptomatic PAD is common among older women”2 meaning that the typical symptoms like claudication, rest pain, diabetes, or exertional leg pain were not present, and PAD could only be discerned through an Ankle Brachial Index blood pressure test (ABI). Physicians do not typically perform this test during regular visits, but you may ask your Primary care, Podiatrist, Gynecologist, or internist if they can perform the test. Effective early detection and treatment of PAD is key to the abatement of the disease.
The article, Sex Differences in Peripheral artery disease from the Women and Cardiovascular Health Compendium speaks about women’s relationship with PAD as well. This article wants to illuminate how PAD affects men and women differently, from how common it is to what causes it, the symptoms, and how to manage it. “PAD affects about 236 million adults around the world, especially older people.”4 Most people don't even know they have it because they don't have any symptoms. “To check for PAD, doctors usually measure the blood pressure in your legs and arms using something called the ankle-brachial index (ABI).”4 There are some differences between men and women when it comes to the ABI values, but changing the definition of PAD can make those differences go away. However, if they set the bar too low, they might miss cases where people have a serious problem.
Women often have unusual symptoms or no symptoms at all, so it's harder to spot PAD in them. The number of women with PAD might be higher than what we think because of the challenges in diagnosing it. “The way PAD shows up in men and women is different because of their blood vessels, hormones, and how they react to stress.”4 One of the first signs of PAD is when the blood vessels don't work properly, and that happens earlier in men than in women. Women start having problems around menopause. Hormones, like estrogen, play a role in this difference.4
Another journal article titled, “A Hidden Problem: Peripheral artery disease in Women” from The European Society of Cardiology examines the existing literature on PAD in men and women through the lens of social constructivism. This theoretical perspective emphasizes the influence of social interaction and cultural context on individuals' knowledge and understanding of the world. The article identifies key themes related to gender disparities in the diagnosis, treatment, and management of PAD, taking into consideration biological, clinical, and societal factors. “Notably, hormonal factors, comorbidities, and associated conditions among women can impact the risk of developing PAD.”5
Differences in the diagnosis and treatment of PAD exist between men and women. Women often have lower awareness of PAD risks, and healthcare providers may overlook the condition in women. “The impact of sex on PAD development involves genetic factors, arterial health, responses to stress, and other factors.”5 Diagnostic criteria may not accurately capture women's symptoms, leading to missed or incorrect diagnoses. Improving knowledge and awareness of PAD among women and healthcare providers is essential. Gender inequalities, including societal biases and women's perceptions of symptoms, contribute to these disparities. Social structures, such as socioeconomic factors and geographical patterns, also influence gender differences in PAD.
More research is needed, focusing on diverse populations and addressing the specific needs of women with PAD. This review emphasizes the importance of considering gender-related factors to address inequalities in PAD. “A comprehensive approach is necessary, integrating biological, clinical, and societal factors to improve healthcare outcomes for all individuals affected by PAD.”5
These three articles highlight similar findings regarding women and PAD. They point out that women are more susceptible to developing PAD as they age and have higher morbidity and mortality rates associated with the disease. Women are also more likely to lack typical PAD symptoms, resulting in underdiagnosis and limited care. Biological factors play a role, with women's smaller vasculature making them more vulnerable to severe PAD and decreased mobility. Hormonal factors, such as estrogen, also contribute to the gender differences in PAD. Clinically, there are disparities in diagnosing and treating PAD in women. Lack of awareness among women and healthcare providers, as well as inadequate diagnostic criteria that may not capture women's symptoms accurately, contribute to underdiagnosis and misdiagnosis. Societal factors, including gender roles and biases, can further exacerbate these inequalities. Women may have different perceptions of pain and may downplay their symptoms, leading to delays in seeking care. To address these disparities, there is a need for more research that includes diverse populations and focuses on the specific needs of women with PAD. A comprehensive approach is necessary, considering biological, clinical, and societal factors, to improve healthcare outcomes for all individuals affected by PAD.
Learn More About Peripheral Artery Disease:
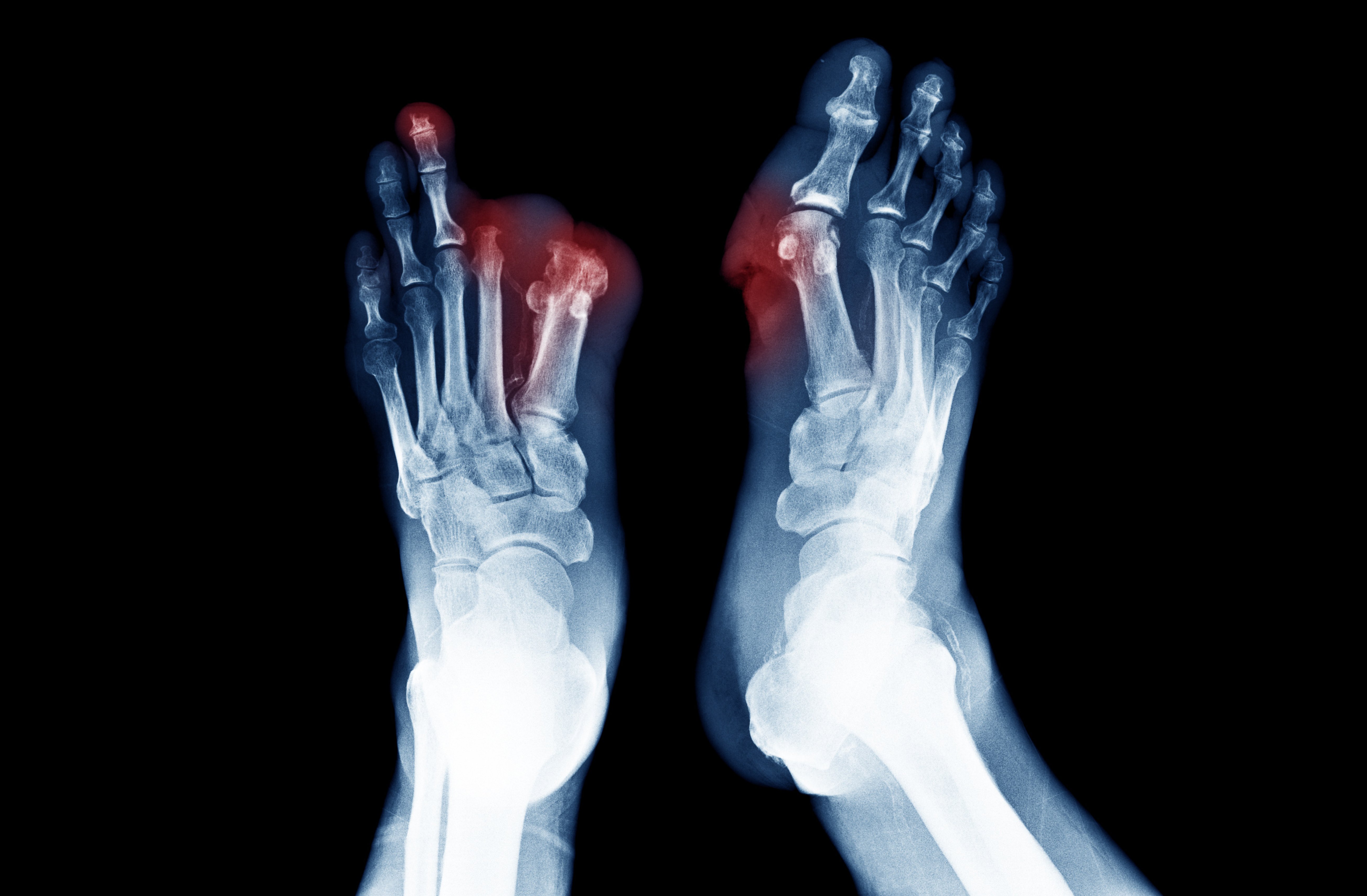
Peripheral artery disease results from the process of atherosclerosis, a build-up of plaque, in the arteries of the legs and feet. Patients with PAD have narrowed or blocked arteries in their lower limbs leading to reduced blood flow that can cause several painful symptoms. If left untreated, PAD can lead to severe consequences such as amputation or death.
Although PAD might develop with advanced age, other factors such as high blood pressure, smoking, diabetes, and genetics can make one more susceptible to the disease.
Individuals with PAD in its early stages may not experience any symptoms or suffer mild leg pain, which can lead to underdiagnosis of the disease. As a result of this underdiagnosis and failure to adequately screen patients, many people with PAD do not receive therapy or have delayed treatment.
Some symptoms that may indicate the presence of PAD include:
Patients experiencing any symptoms of PAD should see a doctor for an official diagnosis in order to prevent serious consequences such as a threatened limb amputation.
How Can Revascularization Help People With PAD:
Many patients are told by their physician that amputation is their only option due to lack of awareness of available treatment options such as revascularization or providers that offer these potentially limb and life-saving procedures. An interventional expert in PAD and limb salvage, comments:
“In my opinion, every patient that has been told they need an amputation should ask for a second opinion.”3
- Dr. Jihad Mustapha
If you suspect you have peripheral artery disease, speak with your physician about all of the available treatment options and preventative measures, and discuss your eligibility for a revascularization.
Recent advances in techniques and devices in revascularization may offer the best treatment option for those who have PAD. The most advanced technology on the market, called Lumivascular technology, allows a doctor to see inside the patients’ artery in real-time during treatment using a minimally invasive approve. The physician can use the image-guidance system to safely remove as much plaque needed to return blood flow through the artery.
Lumivascular Procedure to Help Restore Blood Flow:
Lumivascular plaque removal represents a significant technological advancement that incorporates an image-guidance system on the end of a minimally invasive device. This camera-like visualization allows a physician to see inside the patients’ artery in real time while removing built-up plaque.
Throughout the entire procedure, the physician can clearly see inside the obstructed artery and differentiate between healthy and diseased tissue. Using this information, not available with any other technology in real time, the physician can remove as much plaque as needed to improve blood flow and resolve or improve symptoms.
If you are diagnosed with peripheral artery disease and want to improve the blood flow to your arteries in your lower limbs, ask your doctor about Lumivascular plaque removal. Click here to find a Lumivascular Physician doctor nearest you. If you or a loved one is suffering from the possibility of amputation, take action today and get a second opinion.
If you are diagnosed with Peripheral Arterial Disease and want to improve the blood flow to your arteries in your lower limbs, ask your doctor about Lumivascular plaque removal. Click here to find a Lumivascular doctor nearest you.
Related Articles:
References:
-
Dhaliwal G, Mukherjee D. Peripheral arterial disease: Epidemiology, natural history, diagnosis and treatment. Int J Angiol. 2007 Summer;16(2):36-44. doi: 10.1055/s-0031-1278244. PMID: 22477268; PMCID: PMC2733014.
-
Hirsch, Alan T., et al. “A Call to Action: Women and Peripheral artery disease.” Circulation, vol. 125, no. 11, 2012, pp. 1449–1472., https://doi.org/10.1161/cir.0b013e31824c39ba.
-
Jihad A. Mustapha, Barry T. Katzen, Richard F. Neville, Robert A. Lookstein, Thomas Zeller, LarryE. Miller, Michael R. Jaff. Determinants of Long‐Term Outcomes and Costs in the Management of Critical Limb Ischemia: A Population‐Based Cohort Study. JAHA, 2018 DOI: 10.1161/JAHA.118.009724
-
Pabon M, Cheng S, Altin SE, Sethi SS, Nelson MD, Moreau KL, Hamburg N, Hess CN. Sex Differences in Peripheral artery disease. Circ Res. 2022 Feb 18;130(4):496-511. doi:10.1161/CIRCRESAHA.121.320702. Epub 2022 Feb 17. PMID: 35175843; PMCID: PMC8919803.
- Kavurma MM, Boccanfuso L, Cutmore C, Passam F, Patel S, Hennessy A, Loa J, Figtree GA, Golledge J, Robinson DA, Aitken S. A hidden problem: peripheral artery disease in women. Eur Heart J Qual Care Clin Outcomes. 2023 Mar 8:qcad011. doi: 10.1093/ehjqcco/qcad011. Epub ahead of print. PMID: 36882190.