Topics: Peripheral Artery Disease, Atherectomy, Diabetes, Leg pain, Amputation, PAD Awareness Month, PAD Diagnosis, PAD
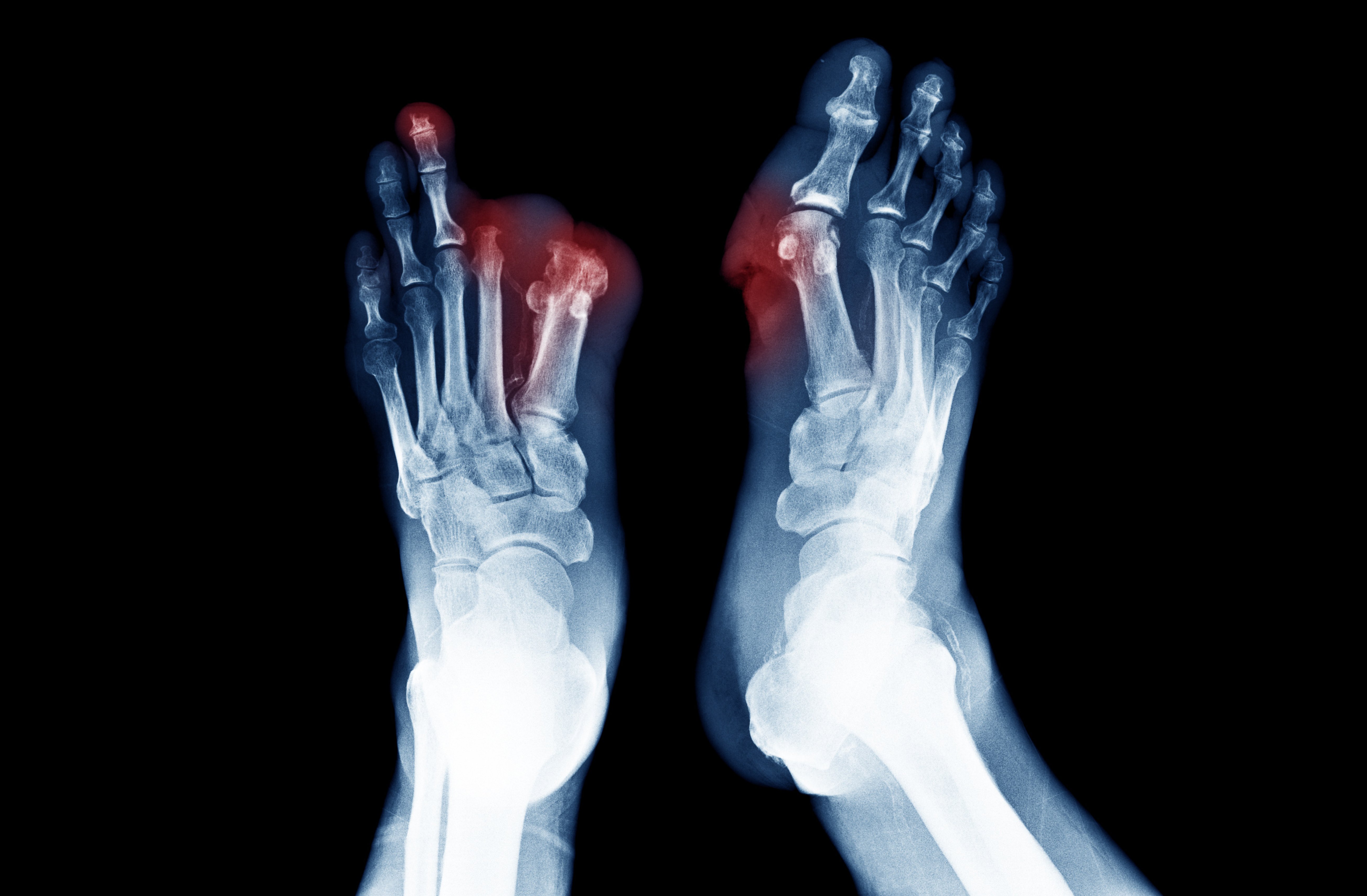
Dr. Olamide Alabi splits her time as a vascular surgeon and researcher between Emory Heart & Vascular Center in Atlanta and the Veterans Health Administration (VHA) Atlanta Healthcare system. Dr. Alabi's dedication to understanding the extent of peripheral artery disease (PAD) and the disparities in preventative care that can lead to Lower Extremity Amputation (LEA) led her to embark on a comprehensive national study. PAD stands for Peripheral Arterial Disease. It is a condition characterized by the narrowing or blockage of arteries, typically in the legs, due to the buildup of fatty deposits (atherosclerosis). This restricts blood flow to the affected area, leading to symptoms like leg pain, cramping, and weakness during physical activity. Severe cases of PAD may result in tissue damage, non-healing wounds, or amputation.

With her dual roles, she possessed a unique perspective that allowed her to approach the study from both clinical and research angles.1 Aware of the staggering number of Americans affected by PAD and the alarming rates of LEAs, Dr. Alabi recognized the urgent need for timely intervention and treatment to hopefully reduce the incidence of amputation. She was determined to uncover the underlying reasons why so many individuals were not receiving adequate screening and preventive care for PAD, leading to devastating consequences.
Given that the VHA is the largest integrated healthcare system in the United States, Dr. Alabi saw an unparalleled opportunity to gather and analyze data on PAD at a national level. She believed that by studying the VHA's patient population, she could gain valuable insights into the disparities and variations in PAD preventative care, which could then inform improvements in clinical practice and healthcare policies.
Dr. Alabi initiated an extensive research project that involved collecting and analyzing data from various VHA medical centers across the country. She and her research team meticulously combed through electronic health records, identifying patients with a diagnosis of PAD and examining their medical histories, treatment patterns, and outcomes. This comprehensive approach allowed Dr. Alabi to capture a holistic view of the disease and its management within the VHA system.
As the study progressed, Dr. Alabi began to uncover patterns and trends that shed light on the factors contributing to delayed or inadequate PAD treatment, including significant disparities in access to screening and preventive care, particularly among underprivileged populations and those living in remote areas. These findings highlighted the urgent need for targeted interventions and outreach programs to ensure that all individuals, regardless of their socioeconomic status or geographical location, receive the necessary care and support.2
Furthermore, Dr. Alabi's study revealed variations in clinical practices among different VHA medical centers, indicating the importance of standardizing protocols and promoting evidence-based guidelines for PAD management. By identifying the best practices and sharing them across the VHA system, Dr. Alabi is working to enhance the quality and consistency of care delivered to patients with PAD.
Throughout her research journey, Dr. Alabi remained committed to bridging the gap between clinical practice and research findings. She actively collaborated with fellow clinicians and healthcare administrators to translate her study's insights into actionable recommendations. Her goal was not only to improve the care provided within the VHA system but also to influence healthcare practices and policies nationwide.1
Dr. Alabi's study on PAD within the VHA system had far-reaching implications for the field of vascular medicine. Her findings not only underscored the urgency of early detection and intervention for PAD but also highlighted the need for healthcare systems to address disparities in access to care. Through her research, Dr. Alabi made significant strides toward ensuring that all individuals at risk of PAD receive timely and appropriate screening, thus reducing the incidence of lower extremity amputations and improving overall patient outcomes.
The Research
Dr. Alabi’s study examines the care provided to veterans with PAD in the Veterans Health Administration (VHA) and explores the factors associated with vascular assessment prior to lower extremity amputations (LEAs). Here are the key points from her research:
- There is substantial variation in the quality and intensity of diagnostic and therapeutic care provided before a subsequent LEA. 2
- Only 35% of patients receive a noninvasive vascular laboratory study prior to LEA, and 54% do not undergo revascularization. 2
- Current guidelines do not recommend routine PAD screening in asymptomatic individuals, who represent the largest subset of those with PAD. 2
- Greater access to primary care and medical specialty care was associated with a higher likelihood of receiving a vascular assessment before LEA. 2
- Veterans with diabetes had a higher likelihood of receiving a vascular assessment. 2
- There was significant geographic variation in the rate of vascular diagnostic and therapeutic interventions provided to veterans.2
- Distance to primary care was associated with the likelihood of receiving a vascular assessment, with veterans living further away being less likely to undergo assessment. 2
The article does not specifically discuss how studying veterans with PAD can directly apply to other Americans who have not served in the armed forces. However, there are potential implications and lessons that can be drawn from studying veterans with PAD that may have relevance for the broader population:
- Understanding healthcare disparities: Studying veterans can provide insights into healthcare disparities and variations in care that may exist in different healthcare systems. By identifying factors associated with disparities in vascular care among veterans, researchers can gain a better understanding of potential disparities in the general population and work towards addressing them.
- Development of best practices: The Veterans Health Administration (VHA) is the largest integrated healthcare system with standardized protocols and guidelines. Studying how vascular care is provided within the VHA can offer valuable information on best practices and approaches that can be applied to other healthcare systems to improve PAD management and reduce preventable amputations.
- Importance of early diagnosis and intervention: Veterans with PAD who received vascular assessments before limb amputations had better outcomes. This highlights the importance of early diagnosis and intervention for PAD in both veteran and non-veteran populations. Implementing early screening and diagnostic measures can help identify PAD earlier and potentially prevent severe complications.
- Impact of access to care: The study touches on the influence of access to care on receiving vascular assessments. Studying veterans can shed light on how geographic factors and distance to care affect healthcare utilization. Understanding these aspects can help healthcare systems develop strategies to improve access to care for all patients, regardless of their veteran status.
- Collaboration between primary care and specialty care: The study emphasizes the role of primary care physicians and specialists in limb preservation efforts. This underscores the importance of a collaborative approach between primary care and specialty care providers in managing PAD and preventing complications, which can be valuable for the broader population as well.
The knowledge gained from studying the veteran population and VHA system can inform healthcare practices and policies that benefit both veterans and non-veterans with PAD. By addressing the unique challenges and disparities faced by veterans with PAD, healthcare systems can work towards improving care and outcomes for all individuals affected by this condition.

How Do You Treat Peripheral Artery Disease?
The treatment for Peripheral Artery Disease (PAD) aims to manage the symptoms, improve blood flow, and reduce the risk of complications. The specific treatment options depend on the severity of the condition and individual patient factors. Here are some common treatments for PAD:
- Lifestyle Changes: Lifestyle modifications play a crucial role in managing PAD. These may include:
- Smoking cessation: Quitting smoking is essential as smoking worsens PAD and increases the risk of complications.
- Exercise: A supervised exercise program, such as walking, can help improve circulation and reduce symptoms.
- Healthy diet: A balanced diet low in saturated fats and cholesterol can help control other risk factors, such as high blood pressure and cholesterol levels.
- Weight management: Maintaining a healthy weight reduces stress on the arteries and improves blood flow.
- Medications: Various medications may be prescribed to manage PAD and its related risk factors, such as:
- Antiplatelet agents: Medications like aspirin or clopidogrel may be prescribed to reduce the risk of blood clots and improve blood flow.
- Cholesterol-lowering drugs: Statins are often used to manage high cholesterol levels and reduce the risk of atherosclerosis progression.
- Blood pressure medications: These drugs help control hypertension and reduce stress on the arteries.
- Peripheral Angioplasty: This is a minimally invasive procedure used to widen narrowed or blocked arteries. A small balloon catheter is inserted into the affected artery and inflated to open the narrowed section. Sometimes, a stent may be placed to keep the artery open.
- Peripheral Arterial Bypass Surgery: In severe cases, when other treatments are ineffective, bypass surgery may be recommended. A blood vessel graft is used to create a detour around the blocked or narrowed section of the artery, restoring blood flow to the affected area.
- Endarterectomy: In this surgical procedure, the plaque buildup inside the affected artery is removed, improving blood flow.
- It involves removing the inner lining of the affected artery along with the plaque buildup.
- Endarterectomy is commonly performed on larger arteries, especially those closer to the heart, such as the carotid arteries in the neck, to treat carotid artery disease.
- During the procedure, a surgeon makes an incision in the artery, exposes the plaque, and carefully removes it along with the inner layer of the artery.
- The artery is then repaired, and the incision is closed.
- Thrombolytic Therapy: This treatment involves using medications to dissolve blood clots that may be causing a blockage in the artery.
- Atherectomy: A minimally invasive procedure used to remove plaque buildup (atherosclerosis) from narrowed arteries. It involves using a specialized catheter with cutting or grinding devices to physically remove or break up the plaque, restoring blood flow through the affected artery.
- Directional Atherectomy: The catheter has a rotating blade at the tip, which cuts and removes the plaque from the arterial wall.
- Rotational Atherectomy: This technique uses a high-speed rotating burr at the catheter's tip to grind away the plaque.
- Orbital Atherectomy: The catheter has a diamond-coated crown that rotates eccentrically to sand the plaque and open up the artery.
It is crucial for individuals with PAD to work closely with their healthcare providers to develop a personalized treatment plan. Early diagnosis and appropriate management can help improve quality of life, reduce symptoms, and prevent complications associated with PAD.
What Avinger Does:
Avinger utilizes its Lumivascular imaging technology as a directional atherectomy procedure to treat PAD. It utilizes advanced OCT imaging technology to guide and assist the physician during the removal of plaque buildup from narrowed or blocked arteries.
OCT stands for Optical Coherence Tomography, which is a medical imaging technique used to obtain high-resolution, cross-sectional images of biological tissues.
During Avinger’s Lumivascular atherectomy procedure, a special catheter equipped with OCT imaging and a stainless-steel cutter is inserted into the affected artery. The imaging technology allows the physician to see inside the artery in real-time, providing a clear view of the plaque and the arterial wall. The cutter removes plaque and stores it in its nosecone to be safely removed from the artery thereby restoring blood flow to the affected artery.
Unlike traditional atherectomy methods that rely solely on X-ray images, Avinger’s Lumivascular atherectomy offers the advantage of direct visualization, which allows for a more targeted and precise removal of the plaque, minimizing the risk of damaging healthy arterial tissue.
Take Action:
If you or a loved one is suffering from the possibility of amputation, take action today. Find a doctor who performs Lumivascular procedures in your area. Lumivascular atherectomy allows your doctor to see inside of your arteries and safely restore blood flow in the affected artery. Improve blood flow in your arteries, find a Lumivascular doctor today.
Literature Cited
- Alexis Hauk. (2023, April 19). Emory-led study examines quality of care for veterans with serious artery disease | Emory University | Atlanta GA. Emory University. Retrieved May 27, 2023, from https://news.emory.edu/stories/2023/04/hs-veterans-peripheral-artery-disease-study/story.html
- Alabi, O., Beriwal, S., Gallini, J. W., Cui, X., Jasien, C., Brewster, L., Hunt, K. J., & Massarweh, N. N. (2023). Association of Health Care Utilization and Access to Care With Vascular Assessment Before Major Lower Extremity Amputation Among US Veterans. JAMA surgery, 158(6), e230479. https://doi.org/10.1001/jamasurg.2023.0479