Topics: Peripheral Artery Disease, Atherosclerosis
 Peripheral artery disease (PAD), which is characterized by atherosclerosis in the arteries of the legs and feet, is underdiagnosed, and undertreated. But what are the risk factors for peripheral artery disease?
Peripheral artery disease (PAD), which is characterized by atherosclerosis in the arteries of the legs and feet, is underdiagnosed, and undertreated. But what are the risk factors for peripheral artery disease?
There are a number of risk factors that predispose individuals to the development of peripheral artery disease—the build-up of atherosclerosis in the arteries. These include, but are not limited to:
Smoking:
Cigarette smoking is one of the most important risk factors for peripheral arterial disease. If you smoke, you significantly increase the risk of PAD by several fold.1-4 In fact, smoking is a more influential risk factor for PAD than it is for coronary artery disease.5
If you smoke, your risk of peripheral artery disease is 4 times greater than that of nonsmokers. In addition, smokers experience onset of PAD symptoms almost 10 years earlier than nonsmokers.6
Also 70–90% of patients with critical limb ischemia are current smokers or ex-smokers.7-9 Critical limb ischemia is the most severe form of PAD and people with it suffer from foot wounds, ulcers, the inability to heal wounds and the risk of amputation. Amputations are also more common in patients who have been heavy smokers.10
Diabetes:
Diabetes increases the risk of developing peripheral arterial disease by up to four times and leads to an increased risk of cardiovascular events and early death. 20% of symptomatic patients with PAD had diabetes,2 but according to the American Diabetes Association, that number is likely much greater.12
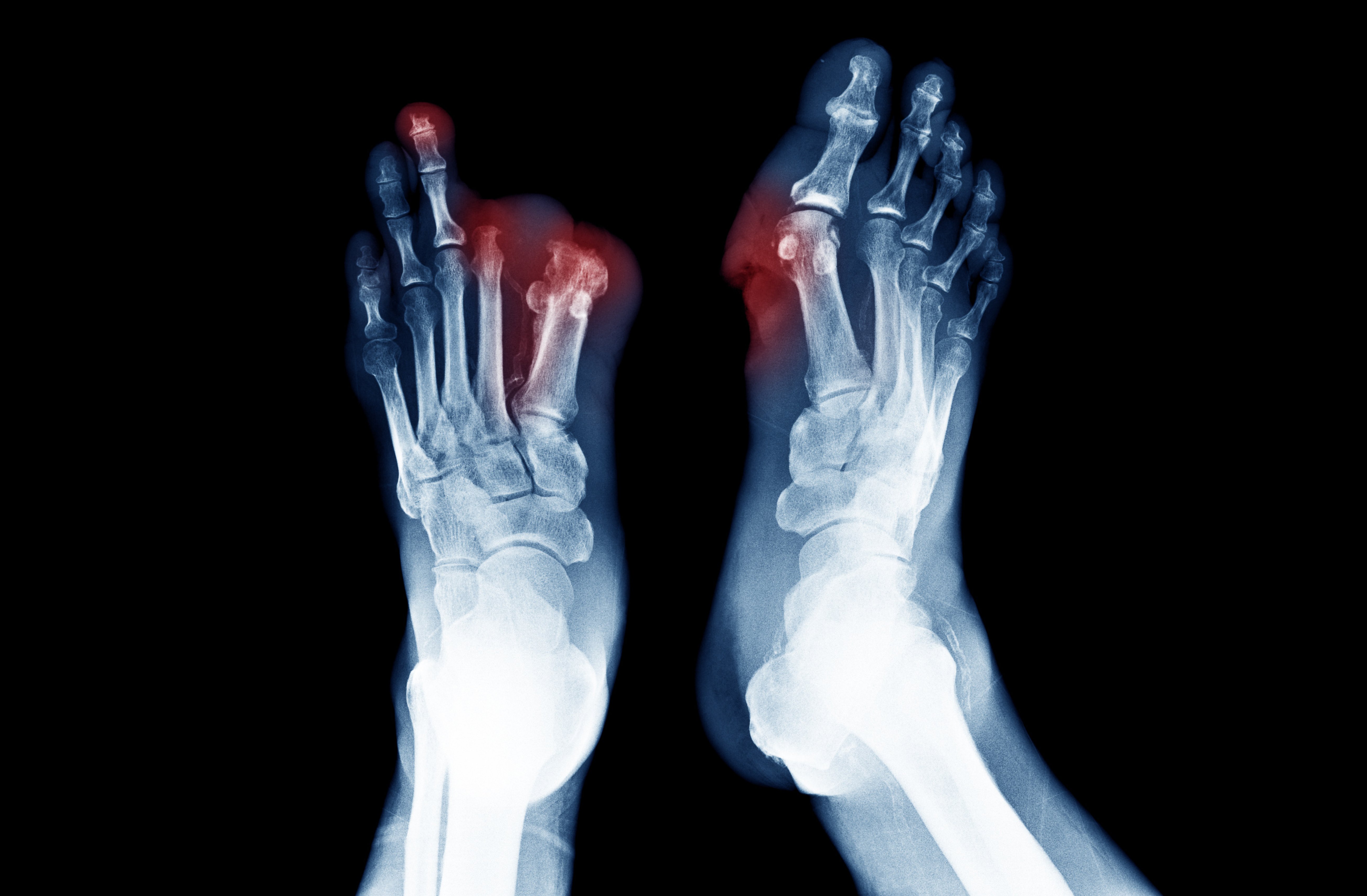
For the diabetic patient, pain perception may be reduced by peripheral neuropathy - a weakness or numbness in hands and feet from nerve damage. This means that a person with diabetes and peripheral arterial disease may only notice the more severe symptoms like an ischemic ulcer or gangrene. Whereas a patient without diabetes may notice the less serious symptoms of PAD earlier.13
Lower-limb ulcers are the most reliable indications of future amputation.14 Patients with Diabetic Foot Disease fear having lower-extremity amputation more than death.15 Of the people with diabetes who have a lower extremity amputation, up to 55% will need to have their second leg amputated within 2‐3 years.16
Additionally, diabetes is a greater risk factor for peripheral artery disease in women than men, and the prevalence of PAD is higher in African American and Hispanic diabetic populations.17-19
If you have uncontrolled diabetes, it considerably increases your risk for peripheral arterial disease and the progression of PAD. Therefore, diabetes control is a very important risk factor for peripheral artery disease.
Older age:
As you get older, your risk for atherosclerosis increases. By the time you're middle-aged or older, enough plaque may build up in your arteries to cause signs or symptoms of peripheral artery disease to begin to show. In fact, research shows that the risk of PAD increases significantly after age 40, rising more than 10% among patients in their 60s and 70s. With aging of the global population, it seems likely that PAD will be increasingly common in the future.20
High Blood Press (Hypertension):
High blood pressure is strongly associated with development of atherosclerosis in general, and peripheral artery disease in particular. As many as 90% of patients with PAD have hypertension.21 Therefore, high blood pressure is a powerful cardiovascular risk factor for PAD as well.
High Cholesterol (Dyslipidemia):
The higher the cholesterol level, the higher the risk of developing peripheral artery disease and coronary artery disease. A study from the Center for Disease Control found that more than 60% of patients with PAD had high cholesterol.22 An elevated cholesterol level was associated with double the risk for chronic leg pain. Treating high cholesterol may reduce risk for peripheral artery disease progression.
Ethnicity:
Peripheral artery disease is more common in African Americans than any other racial or ethnic group. The risk is higher for African Americans because of conditions that increase the risk for developing PAD, such as diabetes and high blood pressure, are more common among this group.23
- An estimated one in four African Americans between the ages of 65 and 74 has diabetes.24
- Compared to other ethnic groups, African Americans have 1.5 times the risk of limb loss due to peripheral artery disease.25
Family history:
People who have a parent or sibling with atherosclerosis have a much higher risk of developing atherosclerosis than others, making it a risk factor for peripheral artery disease. In fact, individuals with a family history of PAD have nearly double the odds of having PAD when compared to those without such a history.26
Metabolic syndrome:
Metabolic syndrome – the combination of obesity, high cholesterol, high blood pressure, and high blood sugar – increases the risk for PAD, as it does for coronary artery disease.27
One study found that Metabolic syndrome greatly increases a woman's chance of developing peripheral arterial disease. According to the data, the risk for developing PAD was 62% higher for women with metabolic syndrome than for those without.28
Chronic kidney disease:
Finally, if you have with chronic kidney disease (CKD) are at a higher risk of developing peripheral artery disease (PAD) and its symptoms compared to individuals with normal renal function.29 Classic atherosclerosis risk factors include age, smoking, diabetes, hypertension and hyperlipidemia. These risk factors are common in chronic kidney disease patients. But chronic kidney disease also impose additional unique risk factors that promote peripheral arterial disease (e.g., chronic inflammation, hypoalbuminemia and a pro-calcific state).
Take Action:
To learn more about Peripheral Artery Disease and treatment options
Find a Lumivascular physician in your area
If you have found this article helpful, please don’t forget to share!
References:
- McGill HC. The cardiovascular pathology of smoking. Am Heart J. 1988;115:250–257.
- Murabito, et al. Intermittent claudication. A risk profile from The Framingham Heart Study. Circulation. 1997;96:44–49.
- Powell, et al. Risk factors associated with the development of peripheral arterial disease in smokers: a case control study. Atherosclerosis. 1997;129:41–48.
- Cole, et al. Cigarette smoking and peripheral arterial occlusive disease. Surgery. 1993;114:753–756
- Li, et al. The Relationship of Cigarette Smoking to Peripheral Arterial Disease. Rev Cardiovasc Med. 2004;5(4):189-193
- Olin, et al. Peripheral Artery Disease: Current Insight Into the Disease and Its Diagnosis and Management. Mayo Clin Proc. 2010 Jul; 85(7): 678–692.
- Hiatt, et al. Effect of diagnostic criteria on the prevalence of peripheral arterial disease The San Luis Valley diabetes study. Circulation. 1995 Mar 1;91(5):1472–9.
- Kannel, et al. Update on some epidemiological feature of intermittent claudication: the Framingham Study. J Am Ger Soc. 1985 Jan;33(1):13–8.
- Kannel, et al. Latest perspectives on cigarette smoking and cardiovascular disease: the Framingham study. J Card Rehabil. 1984;4:267–77.
- Vogt MT, Cauley JA, Kuller LH, Hulley SB. Prevalence and correlates of lower extremity arterial disease in elderly women. Am J Epidemiol. 1993 Mar 1;137:559–68.
- Jensen, et al. The Prevalence of Chronic Critical Lower Limb Ischaemia in a Population of 20,000 Subjects 40–69 Years of Age. Eur J Vasc Endovasc Surg. 2006 Jul;32(1):60-5.
- Clark, N. Peripheral Arterial Disease in People with Diabetes. Diabetes Care 2003 Dec; 26(12): 3333-3341.
- American Diabetes Association Peripheral arterial disease in people with diabetes. Diabetes Care 2003;26(12):3333-3341
- Beckert, et al. A New Wound-Based Severity Score for Diabetic Foot Ulcers. Diabetes Care 2006; 29:988–992
- Wukich, et al. Patients With Diabetic Foot Disease Fear Major Lower-Extremity Amputation More Than Death. Foot Ankle Spec. 2018 Feb;11(1):17-21.
- Pandian, et al. Rehabilitation of the Patient with Peripheral Vascular Disease and Diabetic Foot Problems. In: DeLisa JA, Gans BM, editors. Philadelphia: Lippincott‐Raven; 1998.
- Kannel, et al. Update on some epidemiologic features of intermittent claudication: the Framingham Study. J Am Geriatr Soc. 1985;33(1):13-18
- Smith, et al. Atherosclerotic vascular disease conference: writing group II: risk factors. Circulation 2004;109(21):2613-2616
- Wattanakit, et al. Risk factors for peripheral arterial disease incidence in persons with diabetes: the Atherosclerosis Risk in Communities (ARIC) Study. Atherosclerosis 2005;180(2):389-397
- Crique, et al. Epidemiology of Peripheral Artery Disease. Circ Res. 2015;116:1509-1526
- Ness, et al. Prevalence of Symptomatic Peripheral Arterial Disease, Modifiable Risk Factors, and Appropriate Use of Drugs in the Treatment of Peripheral Arterial Disease in Older Persons Seen in a University General Medicine Clinic. J Gerontol A Biol Sci Med Sci. 2005;60(2):255-7.
- Selvin, et al. Contemporary risk factor control and walking dysfunction in individuals with peripheral arterial disease: NHANES 1999-2004. Atherosclerosis 2008;201(2):425-433
- https://www.nhlbi.nih.gov/files/docs/public/heart/pad_extfactsheet_aa_508.pdf
- Ghidei, et al. African Americans and Peripheral Arterial Disease: A Review Article. ISRN Vascular Medicine. 2012; Article ID 165653, 9 pages doi:10.5402/2012/165653
- Collins, et al. Lower extremity nontraumatic amputation among veterans with peripheral arterial disease: is race an independent factor? Medical Care. 2002; vol. 40, supplement 1, pp. I106–I116.
- Khaleghi, et al. Family history as a risk factor for peripheral arterial disease. Am J Cardiol. 2014 Sep 15;114(6):928-32.
- Oriol Torón, et al. Metabolic syndrome and peripheral artery disease: Two related conditions. Endocrinol Nutr. 2016 Jun-Jul;63(6):258-64.
- Conen, et al. Metabolic Syndrome, Inflammation and Risk of Symptomatic Peripheral Artery Disease in Women: A Prospective Study. Circulation. 2009; 120:1041-1047
- Garimella, et al. Peripheral Artery Disease and Chronic Kidney Disease: Clinical Synergy to Improve Outcomes. Adv Chronic Kidney Dis. 2014; 21(6): 460–471