 Critical limb ischemia (CLI) is a serious form of peripheral artery disease, or PAD. CLI is typically caused by a severe blockage in the arteries of your lower legs. The symptoms of CLI include pain while not moving the legs, ulcers or gangrene.1Because of this, it is considered the “end stage” of peripheral arterial disease (PAD).2
Critical limb ischemia (CLI) is a serious form of peripheral artery disease, or PAD. CLI is typically caused by a severe blockage in the arteries of your lower legs. The symptoms of CLI include pain while not moving the legs, ulcers or gangrene.1Because of this, it is considered the “end stage” of peripheral arterial disease (PAD).2
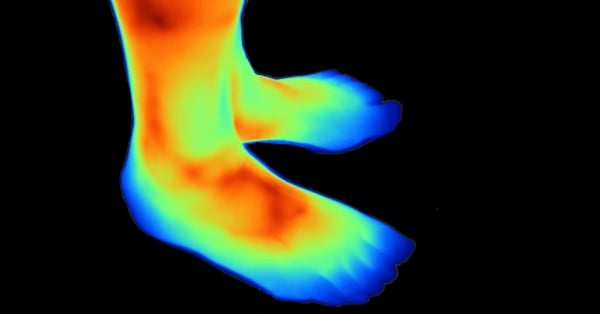
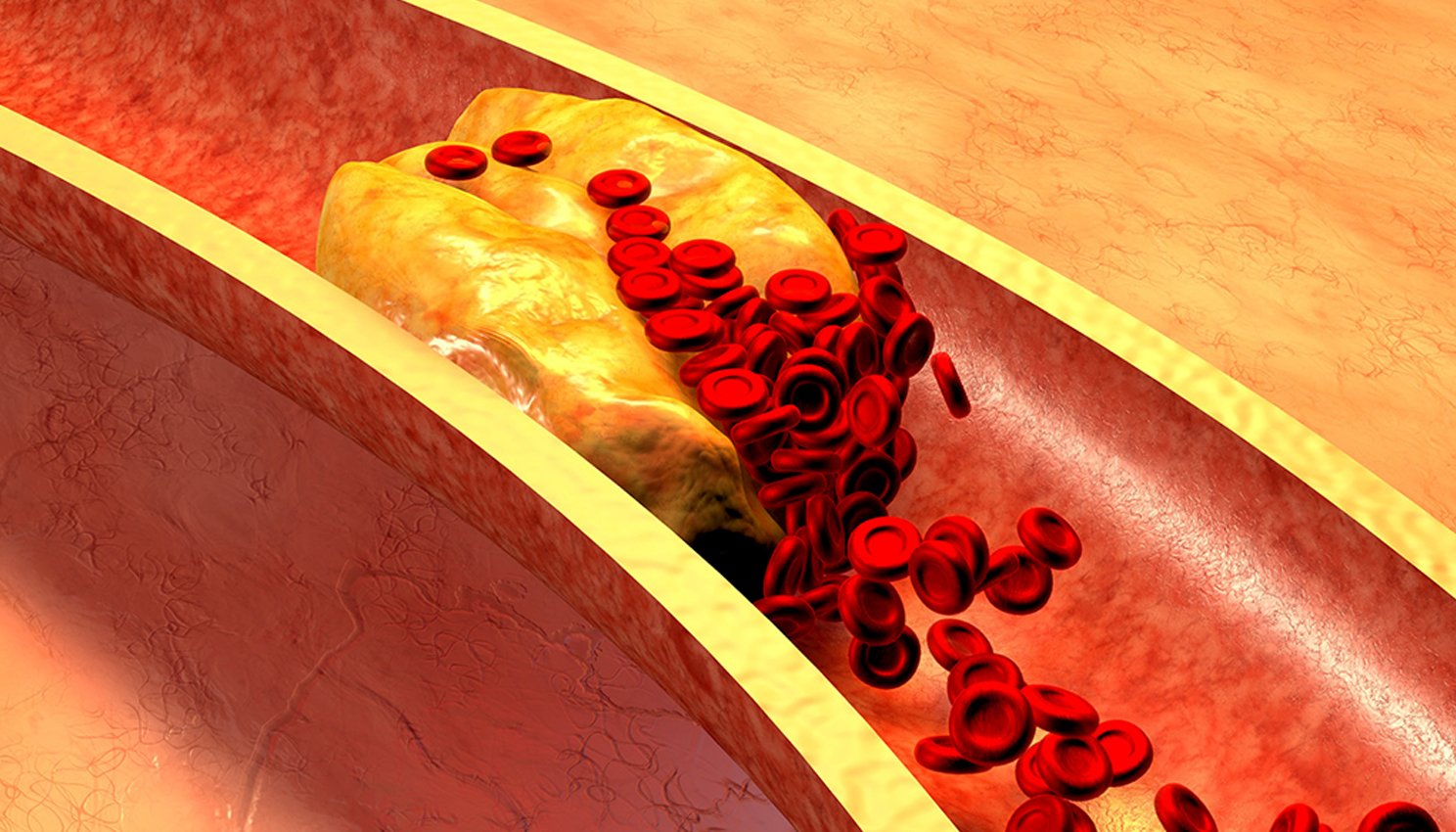
Your body has a complex highway system of arteries that deliver oxygen-rich blood throughout the body. When these pathways get clogged up, it can result in a serious problem called ischemia. In peripheral artery disease, this means your legs and feet are not getting enough blood and oxygen. Critical limb ischemia is a chronic condition and can lead to a cascade of events resulting in rest pain, non-healing wounds, and or ulcers in the legs and feet.
According to an article in Journal of Vascular Surgery, “It is agreed that CLI patients suffer from the worst form of PAD, and approaches to maximize early detection and optimize surgical and nonsurgical therapies should be high priority”.2
Approximately 1% to 3% of patients with peripheral artery disease may present with critical limb ischemia; however, with increasing life expectancy and the prevalence of diabetes, obesity, and sedentary lifestyles, these estimates are likely to increase.3
Critical limb ischemia is a condition that can lead to poorer quality of life and decreased length of life.4 These patients are restricted in physical function and some experience depression.5
 What are the symptoms of Critical Limb Ischemia?
What are the symptoms of Critical Limb Ischemia?
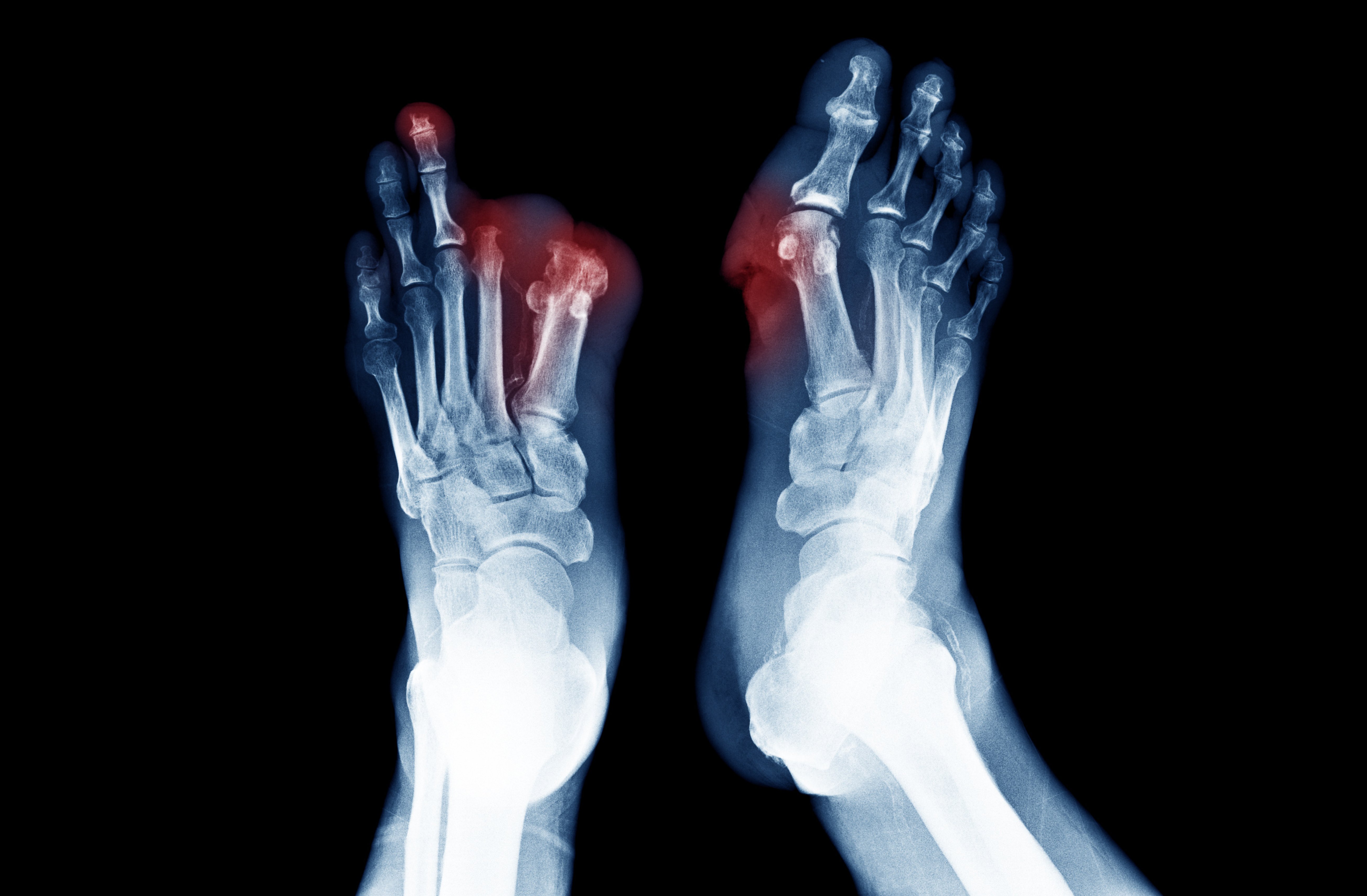
Patients suffering from critical limb ischemia will typically experience severe pain in the legs and feet, even while resting. This pain is known as “rest pain” because it often happens while that patient is resting or asleep. Rest pain can be so severe that it can wake you up at night.
Symptoms of Critical Limb Ischemia include:
- Sudden severe pain
- Loss of pulses
- Coldness of the limb
- Paleness of the skin
- Leg weakness
- Loss of sensation
These symptoms are critical and require immediate medical attention. If left untreated, the critical limb ischemia may result in amputation of the affected limb.
Risk factors of chronic limb ischemia?
Risk factors for chronic limb ischemia are the same for those with atherosclerosis and may include:
- Smoking
- Diabetes
- Advanced age
- High cholesterol
- High blood pressure
- A family history of cardiovascular disease
- Sedentary lifestyle
- Obesity
The first three risk factors are more strongly associated with progressive CLI than others.
Smoking and critical leg ischemia
Smoking is a major risk factor for critical leg ischemia and it is responsible approximately 75% of peripheral artery disease.4 In fact, smoking significantly increases the risk of developing PAD, even more than having coronary artery disease.4
Smoking also adversely affects the myocardial oxygen demand/supply relationship. The toxins found in cigarette smoke cause damage to different biochemical pathways, and together, these injuries can contribute to the worsening of PAD.4
Cigarette smoking is associated with a significant increased risk for atherosclerosis and 70–90% of patients with chronic limb ischemia are currently smokers or ex-smokers.6-9
Additionally, amputations are more common in patients who have been heavy smokers.10
The outcome of critical leg ischemia becomes increasingly bleak if you continue to smoke. One study found that “almost half of the patients will be dead within five years.”11
Diabetes and critical leg ischemia
Diabetes is another important risk factor frequently associated with severe peripheral artery disease. Atherosclerosis develops at a younger age in patients with diabetes and progresses more rapidly. Moreover, atherosclerosis affects vessels in the legs and feet in patients with diabetes. Atherosclerosis in combination with diabetic neuropathy contributes to the higher rates of limb loss in diabetic patients than nondiabetic patients.12
Aging and critical leg ischemia
As you get older, your risk for atherosclerosis increases. Your genes or lifestyle choices can cause plaque to build up in your arteries as you age. By the time you're middle-aged or older, enough plaque can build up to cause signs or symptoms of CLI. Studies show that peripheral artery disease and critical leg ischemia increase significantly after age 40, affecting 21% of people older than 40. It also effects 25% of people 50 plus and 35% of people aged 60 to 69 years.10
The prevalence of chronic critical lower limb ischemia in men and women 40–69 years of age10
The prevalence of chronic critical lower limb ischemia in men and women 40–69 years of age increases by age. As the global population ages, it seems likely that PAD will be increasingly common in the future.
How is critical leg ischemia diagnosed?
Symptoms are typically the first sign of CLI. You doctor may ask you for detailed information such as:
- When and where the pain occurs?
- How often does it occur?
- What relieves the symptoms?
- What exacerbates it?
How is critical limb ischemia treated?
Preserving the limb is the number one priority for patients with critical limb ischemia. CLI patients tend to have severely calcified arteries, which pose a challenge to both the surgical and endovascular revascularization techniques. It requires immediate treatment to re-establish bloodflow to the affected area.
Treatment of CLI depends upon the location of the blockage and its severity. However, for all forms of critical leg ischemia, controlling risk factors, especially stopping smoking, is essential. It may help prevent progression, save your limb or even save your life. Treatment for this is focused on getting more blood supply to your legs and feet. This may be accomplished several ways:
Medications
Medications may be prescribed to prevent further progression of the disease and to reduce the effect of contributing factors such as high blood pressure and cholesterol.
Exercise
If one experiences intermittent cramping in the legs after exercise, a supervised exercise routine may be prescribed. Regular exercise may also result in other benefits such as weight loss, lower blood pressure, lower cholesterol, and better control of diabetes.
Lumivascular Atherectomy – Seeing and removing the blockage
When you develop atherosclerosis, the plaque in your arterties is the problem. Similar to a clogged pipe under your house, you need someone to pull out the debris backing up your pipes. A Lumivascular atherectomy does just that. Through a minimally invasive procedure, your physician can use a guidewire to reach your blockage and remove the plaque with Lumivascular atherectomy. One huge advantage of a Lumivascular atherectomy is that your physician can see inside your vessel! This helps them to see what needs to be removed and avoid injuring any of the healthy lining of your vessels. A major problem with injuring the healthy lining of the vessel is that it may lead to developing blockage again.
Many patients greatly benefit from restoration of blood flow, which is required for wound healing and limb salvage to occur.2 Without revascularization, up to 40% of patients with critical leg ischemia will require lower limb amputation within one year.13
Leg Bypass – Open surgical
A surgical bypass uses a natural or synthetic graft to route blood flow around an area of blockage caused by critical limb ischemia. Another example of a bypass procedure is a coronary artery bypass grafting (also known as CABG or “open heart” surgery). While a bypass can help a number of patients, it is highly invasive and has been shown to have poor outcomes in patients with diabetes.14
Amputation – Removing the limb
When people with peripheral arterial disease are offered amputation for critical limb ischemia, it is usually because there is:
- Iscemic rest pain
- Tissue loss (ulceration, gangrene)
- Infection cannot be controlled by medical therapy
- The doctor feels that the blood supply to the leg cannot be restored
Surprisingly, a doctor may offer and perform an amputation before additional tests are completed.15 If you are offered an amputation, be sure that you talk to your doctor about other options and get a second opinion from a Lumivascular Doctor before committing to amputation.
Endovascular Procedures
A physician may also elect endovascular procedures such as an angioplasty, which is using a balloon to widen the artery, and/or stenting. Using a stent as a scaffolding to keep the artery open can be a viable procedure for some patients.
Conclusion
Chronic critical limb ischemia is a significant atherosclerotic disease that has substantial medical and functional consequences. A thorough understanding of the systemic risk factors associated with the disease accompanied by rapid intervention and interruption of the process is necessary to improve outcomes and prevent limb loss and death.
Patient should talk to your doctor about other options and get a second opinion from a Lumivascular Doctor before committing to amputation.
Learn more about Lumivascular atherectomy
Find a Lumivascular Doctor in your area