Topics: Peripheral Artery Disease, Atherectomy, clogged arteries
April is Limb Loss and Amputation Awareness Month. The purpose of this month is celebrating amputees, sharing the realities of what life after a leg amputation is like, and educating the public on the underlying causes of amputations such as Peripheral Artery Disease (PAD). It is important to recognize that amputation awareness is crucial in saving limbs and lives and that understanding the impact of amputation can help many patients worldwide.
Amputation Awareness Saves Limbs and Lives
With nearly 2 million Americans living with limb loss of which 54% of limb loss is due to diabetes and Peripheral Artery Disease (PAD).1
It is crucial to make people aware of the statistics on amputation so they can take active steps to prevent it. According to the World Health Organization, patients with diabetes are 10 times more likely to have a lower limb amputation than a person without diabetes.2 Because limbs can be saved through preventative measures and alternatives to amputation, awareness is extremely crucial. By promoting the awareness of amputation as a complication due to diabetes and Peripheral Artery Disease, patients can help prevent limb loss.
Patients with diabetes and PAD are at a higher risk for amputation because the symptoms of these diseases can quickly get worse and lead to end stage PAD, known as Critical Limb Ischemia.
“Critical limb ischemia is basically a condition in which there is blockage in the blood vessels of the leg that threatens the life of the leg and puts the patient at risk for amputation,” states Dr. Dwight Dishmon, of Memphis, TN.
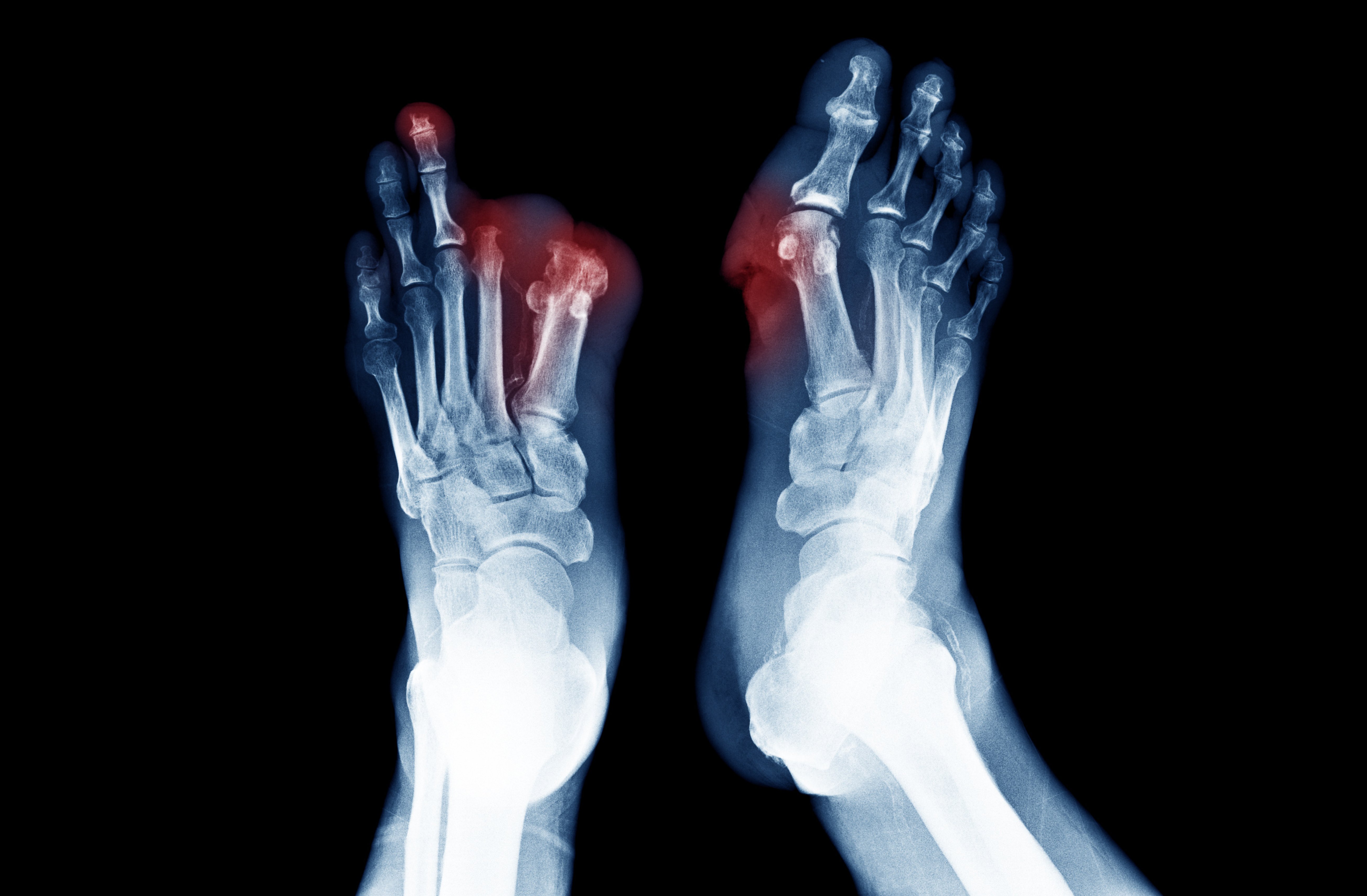
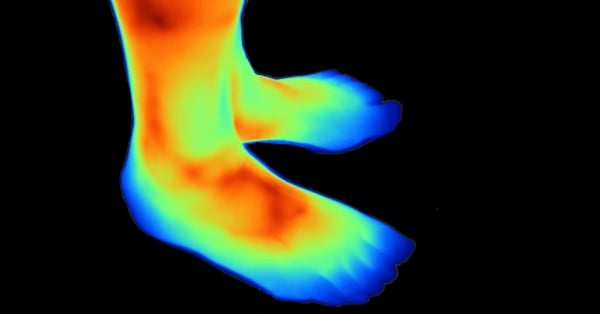
Patients typically notice that their legs have a blueish coloring and are shinier than usual. This changed appearance is because the legs and feet are not receiving a healthy blood flow due to blocked arteries. For patients with Critical Limb Ischemia, they can experience leg pain even at rest.
The reduced blood flow is one of the biggest side effects that can lead to amputation in patients with diabetes and PAD. The poor circulation can actually cause gangrene in the legs and feet of many patients. Gangrene occurs when a body part doesn’t have enough oxygen-rich blood and the healthy tissue begins to die.4 This dead tissue will typically be found on the feet or toes. Patients with diabetes and PAD who have noticed symptoms of gangrene should seek medical treatment immediately because gangrene can quickly lead to amputation.

One major reason why so many patients with diabetes often have their PAD lead to amputation is that it is left undiagnosed and untreated. Peripheral Artery Disease will often go unnoticed in patients with diabetes because of the reduced pain perception they experience because of their peripheral neuropathy. Peripheral neuropathy describes the nerve damage that causes patients with diabetes to have weak or numb feeling in their extremities. This means that patients with diabetes and PAD feel numbness and will not notice the symptoms of PAD until they escalate to the more severe symptoms like non-healing ulcers and gangrene.
Awareness of amputation is crucial for patients with diabetes and Peripheral Artery disease because every 30 seconds a limb is lost to diabetes.5 By better managing their diabetes and PAD, patients can help prevent side effects and complications that could lead to amputation.
Diabetes and Amputation
Amputation due to diabetes is a major concern for many people around the world. It is a common theme that diabetes and amputation go hand in hand but not many people fully understand what causes amputation in diabetics.
So, what causes amputation in diabetics? Well, people who have diabetes have a significant risk of developing Peripheral Artery Disease (PAD) which can cause symptoms that may lead to amputation if not diagnosed or treated correctly.
Many patients suffering from undiagnosed PAD will not see a doctor because they assume their symptoms are arthritis or something else. Self-misdiagnoses are fairly common in patients with Peripheral Artery Disease because the symptoms and the disease itself are not very well known. Additionally, the symptoms may be so minor in some cases that patients wrongly assume that they are fine and do not need to see a doctor.
However, when patients with PAD see a doctor, some professionals may consider amputation as the only solution for the symptoms of poor circulation in the legs or feet that is caused by atherosclerosis (PAD) in the arteries.
This atherosclerosis can lead to gangrene and non-healing wounds in the legs and feet of patients because blood flow is never reestablished. Eventually, these foot wounds and/or gangrene can lead to amputation if not treated in time. “The lack of arterial blood flow will lead to gangrene and/or infectious causes that affect the lower extremities and can lead to amputation,” says Dr. Glen Schwartzberg of Baton Rouge, Louisiana.
Seek a Second Option Before Amputation
However, the problem is that some doctors will jump to the conclusion that patients with Peripheral Artery Disease need amputation without considering the alternative options that can save their limb.
Amputations occur much more frequently than they are needed which can be a serious problem because mortality rates significantly increase for patients after limb amputation.
This is why it is so crucial for anyone with PAD to seek a second opinion before committing to amputating their leg or foot. “You want to get a second, third, fourth, and fifth opinion. You want to get an opinion from someone that treats a lot of CLI.” Says Dr. Tom Davis of Detroit, Michigan. “It really, truly does make a difference.”
Restoring Blood Flow with a Lumivascular Atherectomy
Additionally, patients should also ask their doctor to see if a Lumivascular atherectomy is for them. This procedure will help your doctor see inside of your arteries so they can carefully remove the diseased tissue without removing any of the healthy tissue. For many patients, a Lumivascular atherectomy improved the blood flow to their arteries and prevented the need for limb amputation. But how can you know if you have Peripheral Artery Disease? One of the most prominent symptoms include severe leg pain after walking. Patients with undiagnosed PAD notice that the calves in their legs begin to cramp while exercising which is because of the intermittent claudication of their arteries in their legs.
Additionally, patients with undiagnosed PAD suffer from poor circulation symptoms which makes the leg skin appear blue or shiny due to the blockage in the arteries. They may also notice that their legs feel colder to the touch than other body parts because they are receiving the least blood flow. This poor circulation can actually cause the tissue on the legs or feet to begin to die which can lead to leg amputation surgery if not diagnosed and treated soon enough. If you have diabetes and you notice that you are experiencing any of these symptoms of Peripheral Artery Disease (PAD) and you do not want to risk amputation, a Lumivascular atherectomy may be the best treatment option for you.
If you are diagnosed with peripheral artery disease and want to improve the blood flow in your arteries, ask your doctor if the Lumivascular atherectomy could work for you. Click here to find a Lumivascular atherectomy physician nearest yo
Take Action:
- Patient Story: Watch how Chuck Lyon prevented getting an amputation
- Learn more about Lumivascular atherectomy and Pantheris device
- Find a Lumivascular doctor in your area
Related Articles:
- 13 Fast Facts: Amputation & Peripheral Artery Disease
- Diabetes and Amputation: A Matter of Life and Limb
If you have found this article helpful, please don’t forget to share!
References:
- Ziegler‐Graham K, MacKenzie EJ, Ephraim PL, Travison TG, Brookmeyer R. Estimating the Prevalence of Limb Loss in the United States: 2005 to 2050. Archives of Physical Medicine and Rehabilitation 2008;89(3):422-9
- Boulton AJ, Vileikyte L, Ragnarson-Tennvall G, Apelqvist J. The global burden of diabetic foot disease. Lancet 2005; 366:1719–1724pmid:16291066
- Margolis DJ, Jeffcoate W. Epidemiology of foot ulceration and amputation: can global variation be explained? Med Clin North Am 2013; 97:791–805pmid:23992892
- MacGill, Markus. What you need to know about gangrene. Medical News Today. December 2017.
- International Diabetes Federation and International Working Group of the Diabetic Foot . In: Time to act. Bakker K, Foster AVM, van Houtoum WH, Riley P, editors; The Netherlands: 2005.