Topics: Peripheral Artery Disease

Over 30 million people in the United States have diabetes, and almost one-fourth of those individuals don’t know they have it. The health consequences of untreated diabetes are severe and can be life-altering.1
What is Diabetes?
Diabetes is a non-curable disease, which presents itself in two main types.
In Type 1 diabetes, the body is unable to make insulin - a substance that helps transfer glucose (a form of sugar) from the food you eat into your blood and from there into your cells to give you energy. If the sugar can’t be transferred into your cells it remains in your blood and over time will cause significant, life-threatening health issues. As a result, people with Type 1 must inject themselves with insulin each day. Children and young adults are at risk for Type 1 diabetes.
Type 2 diabetes is the most common form of this disease. The body makes insulin but does not use it very efficiently. While Type 2 diabetes can develop at any age, it is most commonly developed by people over 45 years of age. Type 2 can often be controlled by lifestyle changes such as losing weight and exercising regularly, but many people with Type 2 will have to start taking daily insulin injections at some point.
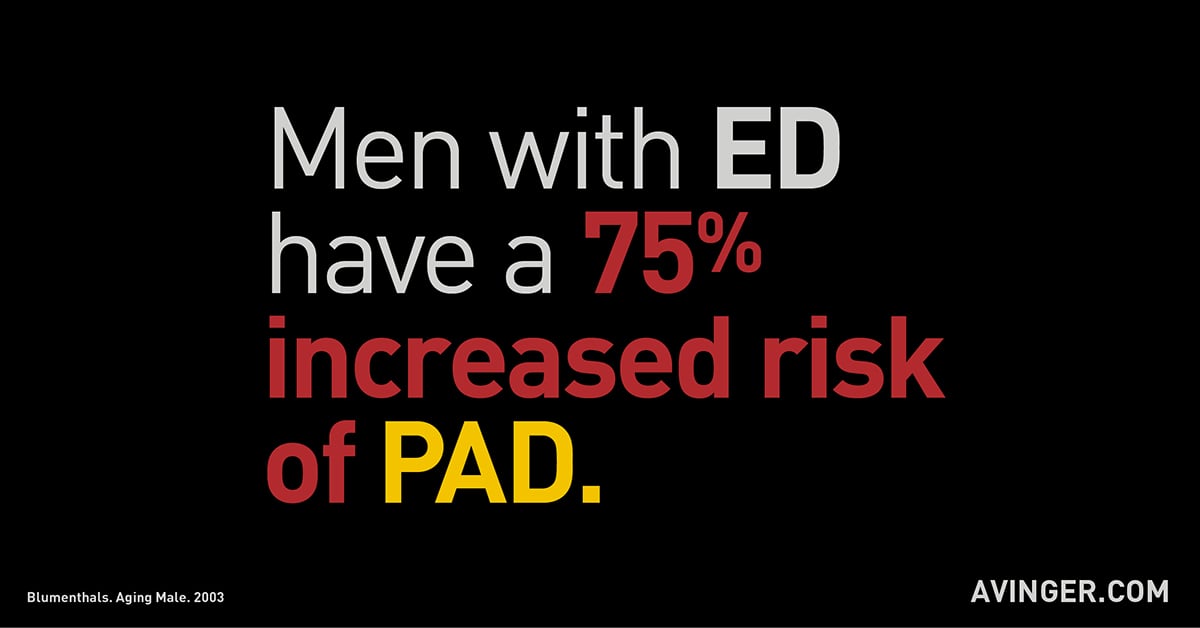
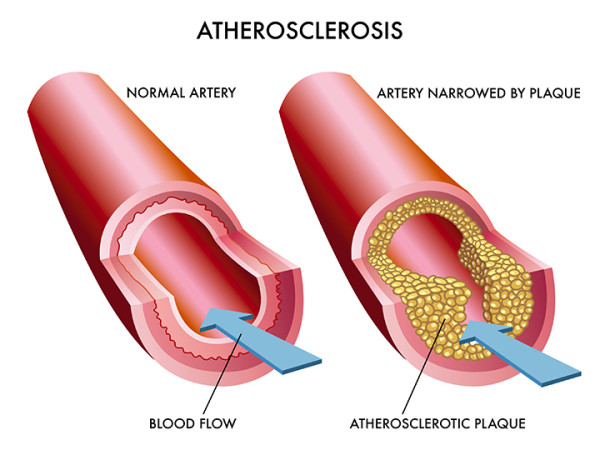
For people with diabetes, the risk of Peripheral Arterial Disease (PAD) is significantly increased. This is because diabetes dramatically accelerates atherosclerosis (hardening and narrowing of the arteries), which is the cause of PAD.2
What is Peripheral Arterial Disease
Peripheral Arterial Disease is a condition similar to Coronary Artery Disease where plaque builds up in the arteries – vessels that deliver blood from the heart to all areas of the body.
PAD targets the legs and feet explicitly. Because the arteries in the legs become narrower and narrower for patients with PAD due to plaque buildup, the flow of blood is obstructed, and can eventually be blocked completely. Without a steady supply of blood, the tissues in the legs and feet can die.
Americans and PAD
Peripheral arterial disease affects approximately 12 million people in the U.S, or 1 in every 20 people,3 with African Americans and Hispanics with diabetes having a higher prevalence of PAD than non-Hispanic caucasians.
Over half of individuals with PAD are asymptomatic, meaning they don’t have the “usual” symptoms, and so they may be misdiagnosed, or they do not report the symptoms they do have to their doctor at all.4
Diabetics and the increased dangers of PAD
It’s estimated that 40% of individuals with PAD have diabetes.5 However, it’s also assumed that that estimate is actually on the low side.
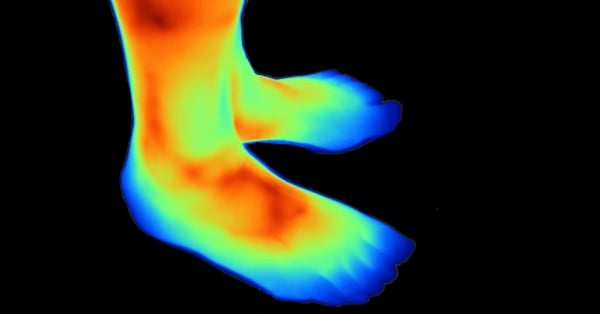
This is because people with diabetes can eventually develop neuropathy – numbness in their fingers and toes. As a result, they often are unable to feel, or they misinterpret, the symptoms of PAD - leg numbness or coldness in the lower leg.
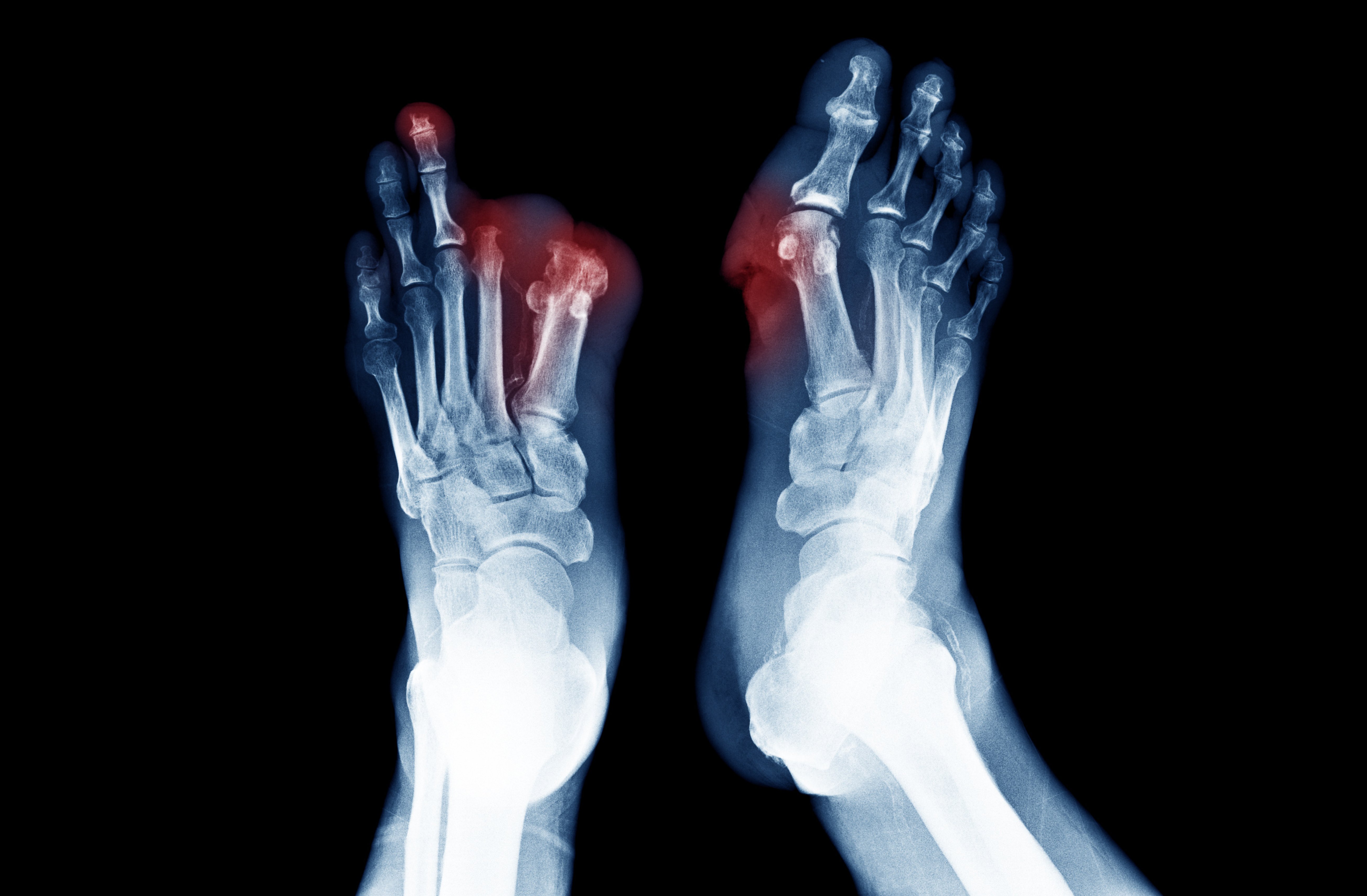
For these reasons, a person with diabetes may not realize they have the condition until a catastrophic event occurs – such as an ischemic ulcer (a wound or sore on the leg(s) or feet, or even gangrene (death of tissue).6
Location of PAD
PAD may occur in the arteries above the knee or below the knee.
For non-diabetics, Peripheral Arterial Disease Above the Knee or “proximal disease in the aorto-iliofemoral vessels” usually presents in individuals with risk factors such as smoking and hypertension.
For people with diabetes, Peripheral Arterial Disease Below the Knee (femoral-popliteal and tibial) is more common. People with diabetes often develop what is called “diabetic foot” – because of numbness in the foot, they are unable to feel any wounds they may have, and so they may not be discovered until they have become infected. About half of people who develop diabetic foot ulcers will also have PAD.
Diabetic foot is a serious condition which may lead to amputation in its most severe form.
Impact of Diabetes and PAD
Approximately 27% of patients with PAD demonstrate the progression of symptoms over a 5-year period, with limb loss occurring in about 4% of these individuals.6
For those individuals who develop Critical Limb Ischemia (CLI), the outcomes are worse: 30% will have amputations, and 20% will die within six months.7
Although the progressive history of PAD in patients with diabetes has not specifically been studied, it has been learned in clinical trials that the cardiovascular event rates (heart attacks) in patients with PAD and diabetes are higher than those that do not have the disease.
According to the American Diabetes Association, “just having diabetes puts you at risk” for Peripheral Artery Disease. Your risk can be even greater if you have the following conditions:
- High blood pressure
- Abnormal blood cholesterol levels
- Overweight
- Not physically active
- Over age 50
- Smoking
- History of heart disease, or you've have had a heart attack or a stroke
- Family history of heart disease, heart attacks, or strokes
By controlling high blood pressure and blood cholesterol levels, individuals can go a long way toward minimizing the likelihood of developing PAD or may be able to slow its progression.
Because obesity contributes to diabetes as well as PAD, it is as well for individuals to work to achieve a healthy weight and then maintain it. This can be accomplished through a healthy diet, and if the individual is mobile, increased physical activity on a regular basis, such as walking or jogging.
For people with diabetes, keeping blood glucose levels as normal as possible is critical. People with diabetes can obtain special footwear to prevent sores, and it is even more critical for them to engage in regular physical activity.
Diabetics with PAD: Diagnosis and Evaluation
The initial assessment of PAD in patients with diabetes should begin with a thorough medical history and physical examination.
This helps to identify those patients with PAD symptoms, such as claudication (cramping while exercising), rest pain (feeling pain while resting), and any functional impairments.
For people with diabetes, development of PAD presents along a spectrum of severity ranging from no symptoms, intermittent claudication, rest pain, and finally to non-healing wounds and gangrene.6
ABI Screening
An ankle-brachial index (ABI) screening measures the blood pressure at the ankle and compares it to that of the upper arm (the brachium). If the blood pressure in the leg is lower, it is evidence of PAD.
A screening ABI should be performed in patients:6
- More than 50 years of age who have diabetes. If results come back “normal," the test should be repeated every five years.
- Less than 50 years of age who have other PAD risk factors (e.g., smoking, hypertension, hyperlipidemia, or duration of diabetes of more than ten years).
Additional tests may include:
- Segmental pressures and pulse volume recording (testing blood pressure)
- Treadmill functional testing (to monitor the function of the heart)
- Duplex sonography (imaging of the tissues)
- Magnetic resonance angiogram (testing the heart)
- Contrast angiography (viewing of the blood vessels and heart chambers)
Medical Treatment for PAD in People with Diabetes
Treatment of the patient with diabetes and PAD should be twofold:6
1) Primary and secondary cardiovascular disease (CVD) risk factor modification.
2) Treatment of PAD symptoms (claudication and critical limb ischemia) and limiting the progression of the disease.
Why Revascularization is important in Diabetes and PAD
Revascularization is a procedure which attempts to restore healthy blood flow to the arteries in the leg and foot to prevent amputation of the limb or extremities.
Before a major amputation is undertaken, revascularization should always be considered and discussed preferably by a multidisciplinary diabetic foot team.7 If you do not have a specialist, you can find one here.
Revascularization
For patients with peripheral artery disease and “diabetic foot,” treating the infection with antibiotics requires adequate blood flow to infected tissues.8 For this reason, a procedure to unclog the arteries can be vital to saving the limb.8
A significant advancement in the treatment of patients with peripheral artery disease and diabetes is image-guided atherectomy with Lumivascular technology. This minimally invasive procedure allows a doctor to see inside an artery so that they can precisely remove plaque that is preventing blood flow. In addition, a Lumivascular procedure helps prevent against vessel injury which has been shown to cause the return of blockage within a year.
Conclusion
- Peripheral artery disease and diabetes are common.
- While leg pain is a common symptom of PAD, the association of peripheral neuropathy may leave many patients with diabetes unable to recognize the symptoms.6
- Patients with peripheral artery disease and diabetes often present later with more severe symptoms.
- The first sign of PAD may be non-healing diabetic foot ulcers and gangrene.
- Patients with PAD and diabetes have a higher risk of amputation.
- Revascularization has been shown to help the healing process associated with PAD and diabetes-related symptoms.
- Image-guided Lumivascular technology can remove plaque and help prevent injury to the vessel.
- Revascularization should be considered before amputation.
If you are suffering the symptoms of peripheral artery disease and diabetes, a minimally invasive Lumivascular procedure can help establish blood flow to your legs and feet. To find a Lumivascular doctor near you, click here to find a doctor.
Take Action:
Find a Lumivascular physician in your area
If you have found this article helpful, please don’t forget to share!
References:
- https://www.cdc.gov/diabetes/pubs/pdf/ndfs_2011.pdf
- Woo, et al. Extracellular signal-regulated kinase 5 SUMOylation antagonizes shear stress-induced antiinflammatory response and endothelial nitric oxide synthase expression in endothelial cells. Circ Res. 2008 Mar 14;102(5):538-45.
- Hiatt, et al. Medical treatment of peripheral arterial disease and claudication. N Engl J Med 2001;344:1608–1621
- Thiruvoipati, et al. Peripheral artery disease in patients with diabetes: Epidemiology, mechanisms, and outcomes. World J Diabetes 2015 July 10; 6(7): 961-969
- Marso, et al. Peripheral arterial disease in patients with diabetes. J Am Coll Cardiol 2006; 47: 921-929
- American Diabetes Association. Peripheral arterial disease in people with diabetes. Diabetes Care 2003; 26: 3333-3341
- Dormandy, et al. Management of peripheral arterial disease (PAD): TASC Working Group: TransAtlantic Inter-Society Concensus (TASC). J Vasc Surg 31: S1–S296, 2000
- Schaper, et al. Specific guidelines for the diagnosis and treatment of peripheral arterial disease in a patient with diabetes and ulceration of the foot 2011. Diabetes Metab Res Rev 2012; 28(Suppl 1): 236–237
- Joseph, et al. Medical therapy of diabetic foot infections. J Vasc Surg 2010;52:67S-71S