Topics: Peripheral Artery Disease, Critical Limb Ischemia, Leg pain, Gangrene, PAD Symptoms, intermittent claudication
Peripheral artery disease (PAD) is a disease where patients have atherosclerosis in the arteries of their lower limbs. This disease is often underdiagnosed and goes untreated because few people understand the symptoms of peripheral artery disease.
There are many symptoms that patients with PAD experience after developing peripheral artery disease. Some patients may experience no symptoms of peripheral artery disease while others will experience just a few symptoms listed below on this list. In fact, nearly 40% of all patients diagnosed with PAD have no symptoms.1 Although there are numerous symptoms of PAD, here are seven of the most prevalent ones.
Leg Pain After Walking

Often, patients who have peripheral artery disease will experience symptoms without realizing it. One of the symptoms of PAD is pain and cramping in the legs while exercising. This pain in the legs with exercise that goes away with rest is known as intermittent claudication.
This leg pain is most often located in the calf muscle of the leg. Patients who have this symptom of PAD will experience this pain in their calf or generalized leg pain while walking. Patients will find that this muscle pain only happens while exercising and the pain will steadily worsen until the patient has to stop because of intolerable pain.
The symptoms of intermittent claudication can affect either or both legs of patients with peripheral artery disease.
Lower Extremity Sores That Will Not Heal
 Non-healing wounds are defined as chronic sores on the lower extremities that do not heal well.2,3 Wounds and sores need a healthy blood supply in order to fully heal. However, patients with peripheral artery disease typically have plaque blocking their arteries and impeding the blood flow to their legs and feet.
Non-healing wounds are defined as chronic sores on the lower extremities that do not heal well.2,3 Wounds and sores need a healthy blood supply in order to fully heal. However, patients with peripheral artery disease typically have plaque blocking their arteries and impeding the blood flow to their legs and feet.
Patients with PAD symptoms will likely notice that their sores will not heal and these neglected wounds could become a very serious problem and require amputation. These non-healing wounds are fairly common as between 500,000 and 2 million people in the United States suffer from leg ulcers, or non-healing wounds.4
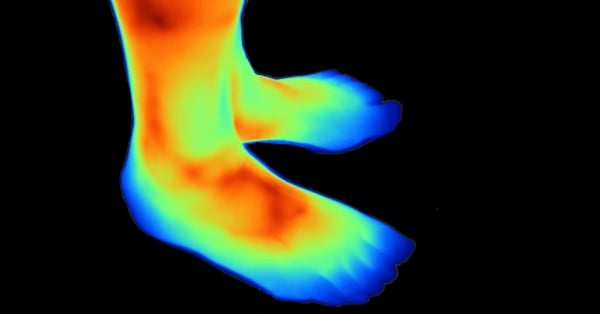
Poor Circulation Symptoms
Another physical symptom of peripheral artery disease (PAD) is any change in the appearance of your legs. Not every patient will experience all of these changes to their legs but these are the ones to look out for.
The skin on the legs many begin to look shiny or the color of one or both of the legs may appear more blueish than before. This blueish color is due to the blockage in the arteries that causes poor circulation symptoms and prevents healthy blood flow to the legs. In addition, patients may find that their toenail and/or leg hair growth has slowed or stopped.
The last change to the legs is that they may feel colder than other body parts. Particularly the toes will feel significantly colder than the rest of the body because they will get the least oxygen-rich blood flow if the patient has undiagnosed peripheral artery disease (PAD). This coldness is also a result of poor circulation to the legs due to PAD.
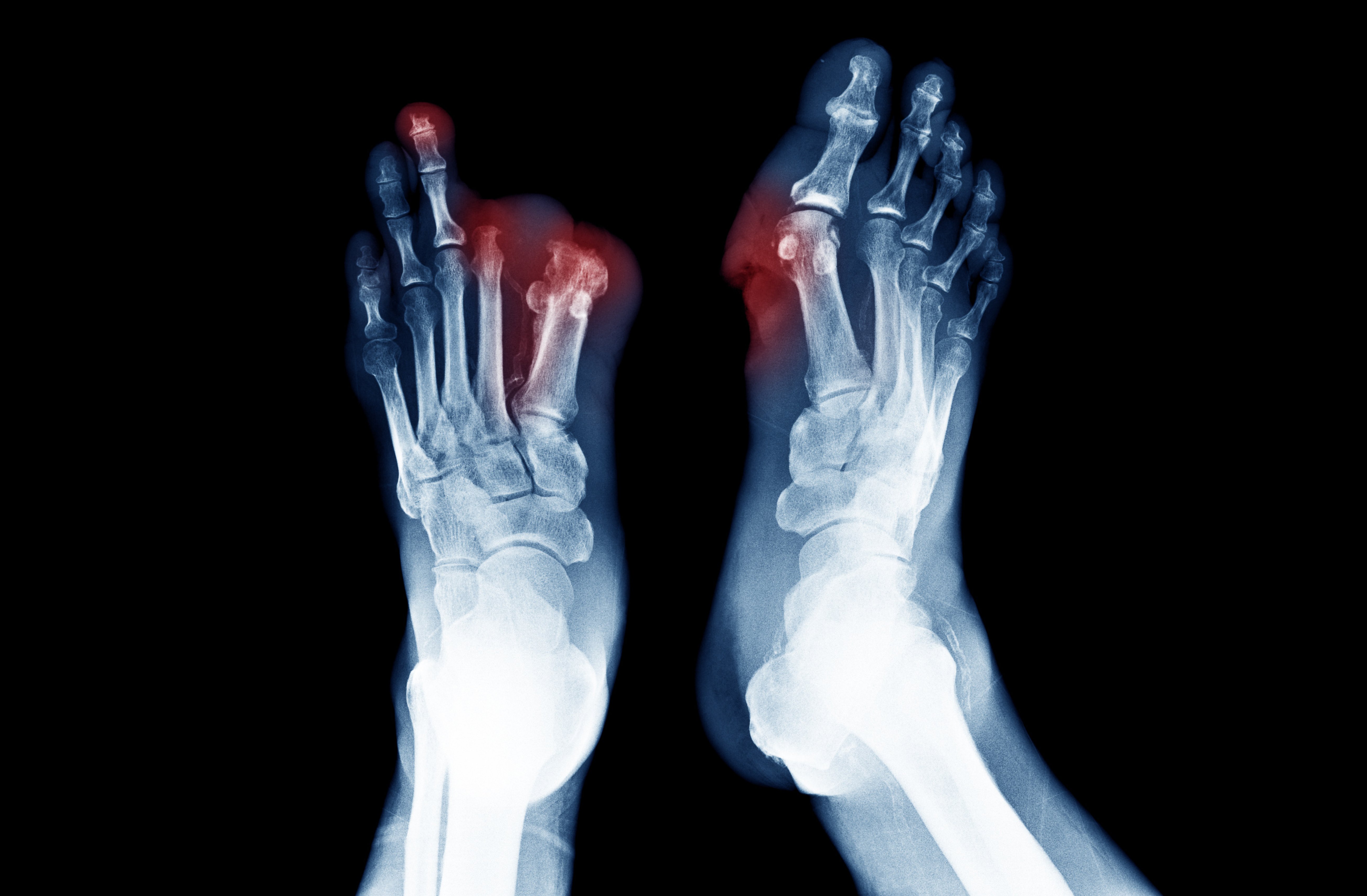
Dead Tissue or Gangrene

Some patients with PAD may notice symptoms of gangrene. Gangrene occurs
when there is a lack of oxygen-rich blood to a body part and some of that tissue begins to die.5
This gangrene will be found in areas of the feet where the blood supply is lost
due to the plaque build-up in the arteries from peripheral artery disease. Patients with symptoms of gangrene will notice this dead tissue or gangrene typically on their toes. If you are experiencing symptoms of PAD-like gangrene, it’s important to get medical treatment immediately as gangrene can lead to amputation of a limb.
Leg Muscle Pain
As patients with undiagnosed PAD get older they tend to attribute their leg pain to a normal sign of getting older. Many patients believe their leg pain comes from arthritis or general stiffness in the legs from aging. However, the difference between other types of leg pain and leg pain as a symptom of PAD is the location. Patients with peripheral artery disease will find that their leg pain is found in their leg muscles and not the joints.6
Critical Limb Ischemia Symptoms
Finally, the most serious stage of peripheral artery disease is known as critical limb ischemia (CLI). Patients with CLI will notice they have severe pain in their lower limbs even while they are resting. This is different than the previously mentioned pain from exercise, because this pain occurs even when the patient did not exercise before resting.
This pain is also called “rest pain” because patients will experience severe pain in their legs and feet while they are resting or asleep. Critical limb ischemia can also cause lower limb pain so severe that it can wake a patient up at night. This is very serious symptom of PAD because if left untreated, 50% of patients with critical limb ischemia will require an amputation or die within their first year.7
Conclusion
If you believe you are experiencing any of these symptoms it is important to talk to your doctor to see if they are symptoms of peripheral artery disease (PAD). If you find that you are experiencing these symptoms of PAD then a Lumivascular atherectomy might be the best treatment option for you. A Lumivascular atherectomy helps your doctor to look inside of your arteries and carefully remove diseased tissue without touching the healthy tissue. If you are diagnosed with peripheral artery disease and want to improve the blood flow in your arteries, ask your doctor if the Lumivascular atherectomy would work for you. Click here to find a Lumivascular atherectomy physician near you.
Take Action:
Find a Lumivascular doctor your area
Patient Stories: Watch how PAD symptoms were resolved
If you have found this article helpful, please don’t forget to share!
References:
- Hirsch, et al. Peripheral arterial disease detection, awareness, and treatment in primary care. JAMA. 2001;286(11):1317-1324.
- Iqbal, et al. Management of Chronic Non-healing Wounds by Hirudotherapy. World Journal of Plastic Surgery. 2017 Jan; 6(1): 9–17.
- Hess, Thomas. Checklist for Factors Affecting Wound Healing. Advances in Skin & Wound Care: April 2011
- Margolis, et al. Venous leg ulcer: incidence and prevalence in the elderly. J Am Acad Dermatol 2002;46(3):381-6.
- MacGill, M. What you need to know about gangrene. Medical News Today. December 2017.
- Gleeson, J. Leg Pain and PAD: Know the Symptoms and Risk Factors. University of Michigan Health. June 2017.
- Davies, D. Critical limb ischemia: Epidemiology. Methodist Debakey Cardiovasc J. 2012 Oct-Dec; 8(4): 10–14.