Topics: Peripheral Artery Disease, Critical Limb Ischemia, Leg pain, Gangrene, intermittent claudication, Poor Circulation
Introduction
Dr. Golzar is on the cutting edge of peripheral arterial disease (PAD) treatment. As an interventional cardiologist with Advocate Medical Group in Chicago, he has helped patients regain their lives by reducing leg pain, reversing gangrene and most importantly, preventing amputations. Dr. Golzar currently maintains a part-time clinical practice and serves as Avinger’s Chief Medical Officer.
Join us as we sit down Dr. Golzar to get his insight about PAD and treatment with Lumivascular technologies.
What is peripheral artery disease?
It's a really good question, and sometimes it's really misunderstood. When we think about peripheral arterial disease, the other word for it is poor circulation. Just like you have blockages in the blood vessels that supply the heart, you can also get blockages in the blood vessels that supply the legs, and this has to do with cholesterol buildup within those blood vessels that prevents the blood to get down to the leg. This can cause pain, gangrene, and can also lead to amputation.
What is atherosclerosis?
Atherosclerosis is the buildup of plaque within the blood vessels. This usually has to do with buildup of cholesterol as the blood vessel gets damaged over time. So, in this situation, what happens is this narrows the blood vessel and causes poor circulation in the legs, which leads to amputation and limb loss.
How does a blood vessels get damaged?
There are multiple risk factors that cause poor circulation, and this is really caused by diet, lack of exercise, high blood pressure, diabetes, smoking cigarettes, poor diet, which consists of high fat diet, high cholesterol diet. This is what causes the inflammation within the cell. Once that blood vessel is inflamed, then it soaks up cholesterol, and that's what then leads to buildup of plaque.
What are the signs of Peripheral Artery Disease?
There are many signs of peripheral arterial disease. Most of the time, peripheral arterial disease is asymptomatic, so you don't even know that you have it. As cardiologists, we see blockages in the heart all the time, and it can be asymptomatic as well. So, it's really important to try to identify patients that are asymptomatic, meaning they don't have any symptoms, because they're still at risk. However, over time, as blockages get worse, you can start having pain in the calves when you walk. This is what we call claudication. The next stage is what we call rest pain, meaning pain occurs even when you don't walk. You have tightness and squeezing and heaviness in the feet, and then, unfortunately, if it still goes untreated, it can lead to sores and ulcers and gangrene, which can eventually lead to amputation.
“It's really important to try to identify patients that are asymptomatic, meaning they don't have any symptoms, because they're still at risk.”
Who should I see about Peripheral Artery Disease?
If you suspect that you have peripheral arterial disease, it's really, really important that you seek medical attention. The best thing to do is go to your primary care physician first and tell them about your concerns, tell them about your symptoms, and it's really important to be aware of what are your symptoms. How far can you walk before you start to have pain? How long has that been going on? These are all the clues that your primary care physician will look for. Then, initially, they can start with non-invasive testing called ABI or arterial duplex. This will be the first stage and will help them understand how much blockage you have and what the level of risk is. If the blockage is at a stage where you need further specialized care, then they will refer you to an endovascular specialist like myself for further treatment.
If my loved-one has been experiencing leg pain for a year or two, and they think it's just kind of a normal part of aging, what would you tell them about getting examined or treated sooner than later?
Spouses of patients are very, very important, because they are the ones that can really encourage that patient and make them go to the physician, because we like to ignore our symptoms because we're in denial sometimes, because we're afraid of what we're going to find. But it's really important to know that now we have such great treatments that we can help you; we can help patients that have poor circulation to prevent you from getting to that stage where you're going to need an amputation. That's the last thing we want to do. So, encourage your spouse, your wife or your husband, to get medical care. Really, if you think it is, if you don't think it is, whatever it is, just get it checked out, because that's the best thing to do.
What's the definition of intermittent claudication?
The definition of intermittent claudication is tightness and pain in the calves when you walk that goes away when you stop walking. So, this means that the muscles in your legs are not getting enough blood flow when you're actually exerting yourself. So, then, that's your body telling you that there's something going wrong, there's a problem. That's why you experience pain, and then, when you stop, then that pain goes away because the blood flow restores to your legs. That's intermittent claudication.
“That's your body telling you that there's something going wrong, there's a problem.”
What is the definition of critical limb ischemia?
When we think about critical limb ischemia, we think about a critical threshold that the leg has reached that it's not getting enough blood flow to be sustainable, to survive. That's your body trying to tell you that there's a major problem. So, when we think about critical limb ischemia, we're thinking about ... It's a stage between rest pain, meaning you have pain all the time, which is different than intermittent claudication, which means you only have pain when you walk.
When you have rest pain all the time, that means you are not getting blood flow. You really need to get immediate attention. The next stage after that is gangrene and ulceration, and again, there's still possible ... Just because you have gangrene doesn't mean you're going to lose your leg. So, it's really important not to be in denial and really to try to seek medical care because we can still save your legs, but at that stage, that means it's a serious, serious condition.
Is PAD Leg Pain similar to angina of the heart?
Leg pain and claudication, critical limb ischemia is very, very similar to angina of the heart. When you think about the physiology behind it, it's very similar. When you heart blockages, you get pain in the heart when you walk because you're not getting enough blood flow to the heart, and so that's your body telling you that there's something wrong. Similarly, in the legs, when you walk and you have pain, that's your body telling you you're not getting enough blood flow to your legs.
Now, the next stage, the critical limb ischemia, is similar to having a heart attack. When you experience 100% blockage, that blockage in your heart, that goes from 70%, 80%, to 100% and you're having a heart attack, then you start having pain all the time and you have tissue loss. You can have congestive heart failure. Similarly, in the legs, when you have constant pain, it's reached that threshold, which means that you're really in serious condition, that you really have to seek medical help.
How do you treat Peripheral Artery Disease?
In terms of treatment options, we have so many treatment options now. Over time, we've had significant progress in the treatment of peripheral arterial disease. If you're asymptomatic and we identify peripheral arterial disease, what we think about is risk factor modification, meaning we want to help prevent you from progressing these blockages. So, diet, good diet, and your physician can talk to you about what that means. Exercise, cholesterol medications, risk factor modification in terms of controlling your diabetes, controlling your blood pressure. That's the initial stages if you don't have symptoms. If you don't have symptoms, you don't need surgery, you don't need any kind of procedures to open the blockage.
However, if you progress to a stage where you do have symptoms of claudication, pain in the legs when you walk, or gangrene, we have multiple options. We have endovascular options where we actually go inside of the blood vessel and clean out your own blood vessel. Very minimally invasive procedure. It's usually done as an outpatient, and it's done under x-ray therapy, and we get it cleaned out, and you can go home same day or next day. If it's at a stage where we can't open with endovascular therapy, then we may consider surgical bypass, but we leave this for a later stage.
What is an atherectomy?
So, when we think about treating peripheral arterial disease, there's many ways to treat these blockages. The older way is to just perform balloon angioplasty. This is the old, traditional way. Then, it progressed to stents, stent implantation. However, we really don't like to leave anything behind, and that's usually the thought process now. So, atherectomy was developed in order to clean out the plaque without damaging the blood vessel. There's a lot of different atherectomy devices, and they all do something a little different. The interesting thing about atherectomy is you can actually remove that plaque from your body and not have to worry about implanting a permanent stent.
What is a Lumivascular atherectomy?
Traditionally, when we do endovascular procedures, we use x-rays, and so we use fluoroscopy, and we see the blockages and we can open them. But we've never been able to actually look inside of the blood vessel to be able to treat the blood vessel, and it's really been groundbreaking, because now we can actually look inside of the blood vessel as we're treating, as we're crossing the blockage, and really direct our treatment to make sure that we remove only the plaque and not damage any normal tissue, because once you damage normal tissue, then you can cause other problems, which is these blockages coming back. Damaging the normal tissue can also cause an inflammatory response, which can have its own issues. So, with lumivascular therapy, you have directed therapy looking just at the plaque, and really, it's been a groundbreaking treatment.
It's really been groundbreaking, because now we can actually look inside of the blood vessel as we're treating.
Related article: What is a Lumivacular Atherectomy?
What is the advantage of seeing inside an artery?
The advantage of seeing inside of the blood vessel, it opens up a whole new world of how we treat patients, because before, we could only see these similar to an x-ray. When you see an x-ray, you're just seeing that anterior, posterior view. Now, you can actually look inside, you can turn your camera around, see 360 degrees, and again, clean out only the plaque and leave the normal tissue behind.
If I have a non-healing ulcer, how important is restoring blood flow?
If you have an ulceration and if you don't restore the blood flow to the foot, you have a very, very high likelihood of amputation, because when you're not getting blood flow to the foot, that foot is going to die, and you have to amputate at the level of where the blood flow is. So, it could be that maybe you just have gangrene of the toe, but if your blockage starts at the thigh level, you would have to have an above-the-knee amputation. That's why it's so important to restore the blood flow to help prevent an amputation, because we know that once you have an amputation, the likelihood of you walking is very, very small. The likelihood of you being functional is very, very small, and the risk of dying from that amputation is very, very high. So, it's really important to restore the blood flow and prevent amputation.
“When you're not getting blood flow to the foot, that foot is going to die.”
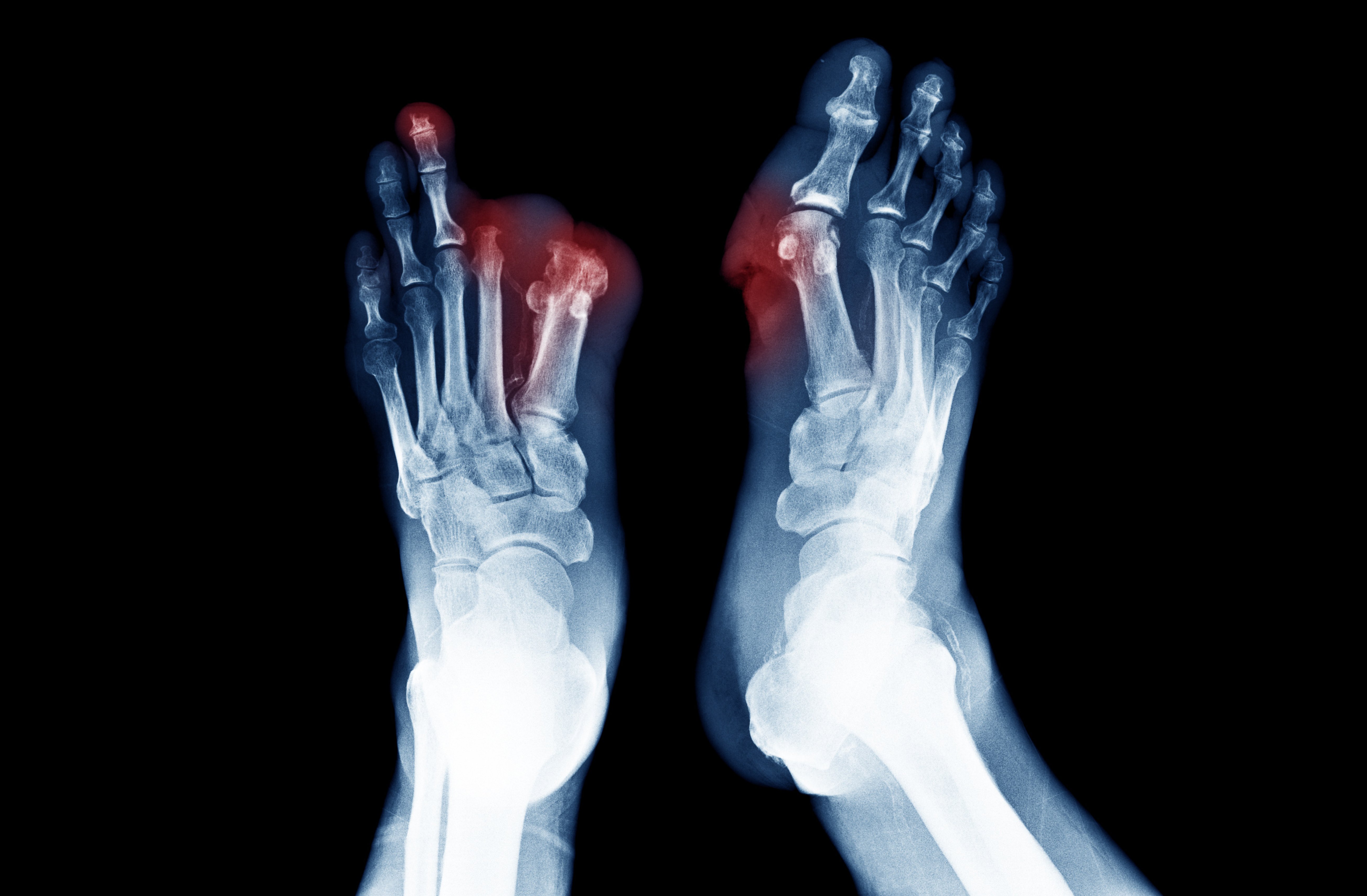
What's the causes of gangrene?
The causes of gangrene are usually due to poor circulation. You're not getting enough blood flow to the foot, and the tissue in the foot starts to die. Usually, you see this either in the toes or in the heel. This is going to be the beginning of what you'll see. It'll usually start with a small ulceration, and then it'll turn black, and it almost looks mummified, because it's dead tissue. When you're not getting blood flow to the tissue, it's going to die. That's going to be what you'll see. If you start to smell a foul odor, that means there's an infection, and that's a medical emergency. So, regardless, if you see any ulceration or gangrene, you really, really need to seek medical care immediately.
If I'm a caregiver, what should I be looking for to know if my loved one has PAD?
If you're a caregiver and you have a family member that has heart disease, that has previous bypass surgery, or maybe they have just high blood pressure, diabetes, or maybe just a smoker, it doesn't matter, there's a lot of risk factors that can cause poor circulation. But if your loved one is complaining of tightness or squeezing the calves when they walk, or they're complaining of rest pain in the foot, or if you start to see an ulcer in the leg, or an infection, please get medical care immediately, because this cannot only save their limb, but also save their life.
Should you get a 2ndopinion before amputation?
If you've been told that you need an amputation without having an angiogram, without having an attempt at opening up that blockage, stop. Walk away. Because there's always another option. In the institution that I practice, we've reduced our amputation rates from 33% to 1.6%, just by working together as physicians and increasing awareness and trying the best we can to prevent that amputation. There's a lot of needless amputations that still go on today, and that is what we have to be aware of, and that's what we're trying to do at Avinger, is to increase patient awareness, to make sure that they know that if you are faced with an amputation or your loved one is faced with an amputation without even attempting to revascularize or opening up the blood vessel, or saving that leg, stop and get a second opinion.
"If you are faced with an amputation...stop and get a second opinion.”
Related Articles:
What is Critical Leg Ischemia?
What is a Lumivacular Atherectomy?
Find a Lumivascular physician in your area
If you have found this article helpful, please don’t forget to share!