Topics: Peripheral Artery Disease, Atherectomy, Diabetes, Leg pain, Amputation, PAD Awareness Month, PAD Diagnosis, PAD, sleep
September is Peripheral Artery Disease (PAD) Awareness Month, so it is a perfect time to discuss the significant role diet plays in achieving a long and healthy life, particularly when it comes to cardiovascular health. While living healthily may pose its challenges, a well-balanced diet is crucial in promoting heart health. If you are living with a cardiovascular condition, you might be wondering whether a specific diet could positively impact your cardiovascular health. We are going to explore some of the popular diets that have been associated with potential benefits for cardiovascular well-being. By understanding the potential impact of these diets, individuals with cardiovascular conditions can make informed choices to improve their overall health and well-being.
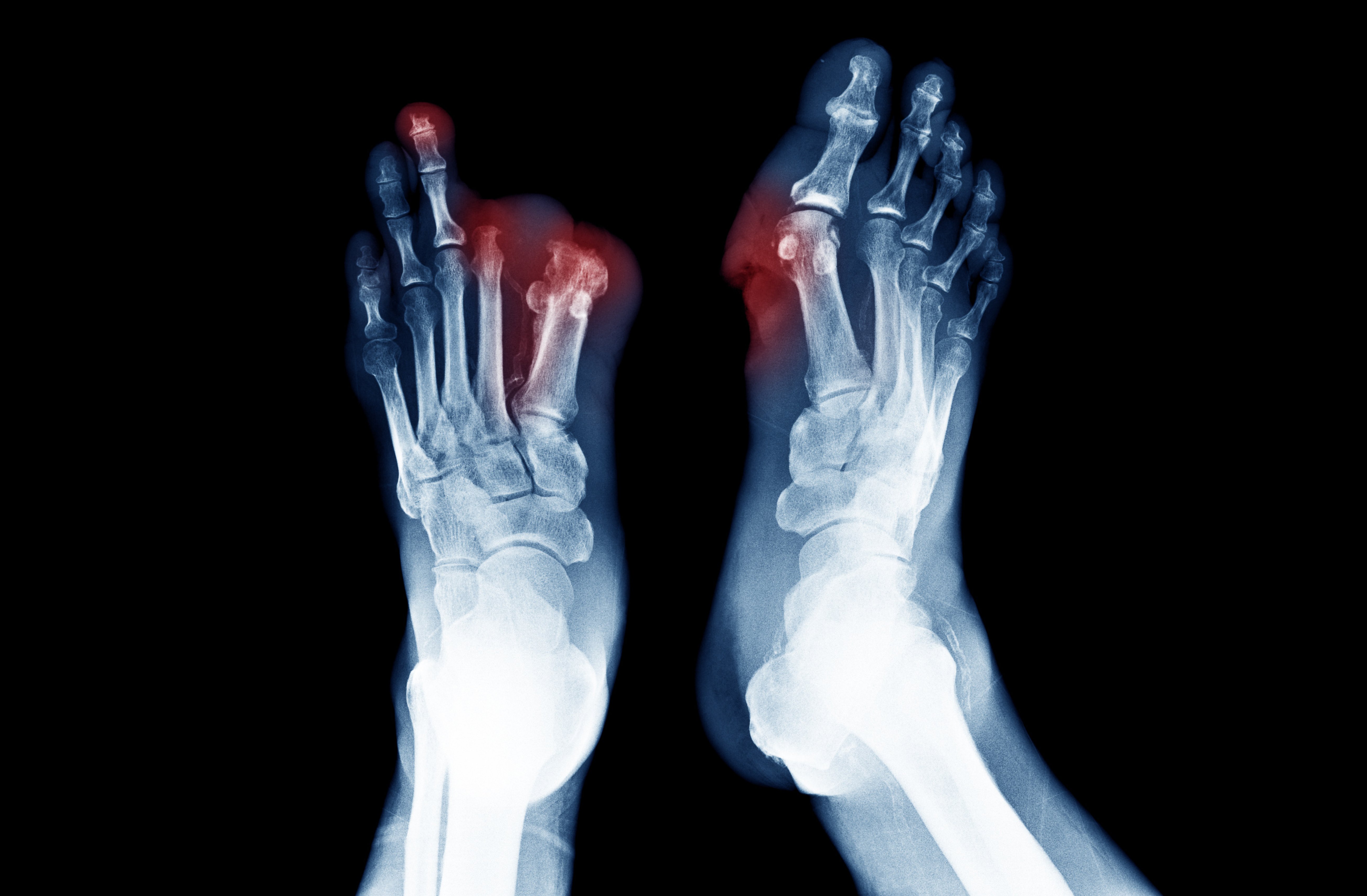
Atherosclerosis is a global health issue causing reduced blood flow to peripheral tissues. PAD is a type of atherosclerosis affecting arteries outside the heart and brain, resulting in severe damage. It is characterized by the narrowing or blockage of blood vessels particularly in the legs, leading to symptoms such as leg pain, muscle cramping, limb numbness and weakness, and slow-healing wounds on the leg and foot. It is an important condition to address as it increases the risk of complications such as infections, ulcers, and in severe cases, gangrene or limb amputation. While medication and medical procedures are often used to manage PAD and improve blood circulation in the affected limbs, an often overlooked way to manage this condition is through diet.1

If you have genetic, environmental, or behavioral factors that make you more susceptible to cardiovascular disease conditions then your diet is critical in preventing major health complications. Unhealthy cholesterol levels and unhealthy lifestyle habits exacerbate atherosclerotic conditions such as PAD.
A study published recently in the International Journal of Molecular Sciences took a deeper look at the way nutrition affects atherosclerosis by examining how four specific diets affect PAD. The four diets studied were a Mediterranean Diet; a Vegetarian, Vegan, and Plant-Based Diet; a Low-Carbohydrate Ketogenic Diet; and an Intermittent Fasting Diet.
- A Mediterranean Diet
A Mediterranean diet is renowned for its remarkable cardiovascular benefits, and researchers have studied its positive impact on heart health. By following this traditional eating pattern inspired by the Mediterranean region, individuals can significantly reduce their risk of heart disease and stroke. The diet's emphasis on whole, unprocessed foods such as fruits, vegetables, whole grains, nuts, and fish provides a plethora of heart-healthy nutrients, including antioxidants, fiber, and omega-3 fatty acids. This combination contributes to improved cholesterol levels, with an increase in HDL (the "good" cholesterol) and a decrease in LDL (the "bad" cholesterol).
The use of heart-healthy olive oil as the primary source of fat helps lower blood pressure, and the anti-inflammatory properties of the diet aid in reducing overall inflammation, benefiting the cardiovascular system.1 Additionally, a Mediterranean diet's balanced approach and focus on nutrient-dense foods contribute to weight management, another key factor in heart health. The MD is considered a non-drug therapy by the American College of Cardiology and the American Heart Association to promote cardiovascular health.1
With its protective effects against blood clot formation and its ability to stabilize blood sugar levels, this diet becomes a formidable ally in preventing cardiovascular complications. By embracing a Mediterranean diet, individuals not only nourish their bodies but also actively promote long-lasting heart well-being and overall health.
A study from The New England Journal of Medicine stated, “persons at high risk for cardiovascular events, those assigned to an energy-unrestricted Mediterranean diet, supplemented with extra-virgin olive oil or nuts, had a lower rate of major cardiovascular events than those assigned to a reduced-fat diet. Our findings support a beneficial effect of a Mediterranean diet for the primary prevention of cardiovascular disease.” 7 Another study also found that, “a Mediterranean diet supplemented with virgin olive oil or a mixture of nuts resulted in lower blood pressure, improved lipid profiles, decreased insulin resistance, and reduced concentrations of inflammatory molecules.”8
Following a Mediterranean diet has been associated with significantly lower incidence of complications and improved survival rates for PAD patients, possibly from such physiological effects as reducing inflammation, managing diabetes, lowering blood pressure, and aiding in weight loss for obese individuals.

- a Low-Carbohydrate Ketogenic Diet
The low-carbohydrate ketogenic diet involves reducing carbohydrate intake and increasing protein and fat consumption to promote fat metabolism and the production of ketone bodies. The diet leads to rapid weight loss, improved glycemic control, and potential reductions in insulin therapy for diabetic management. It also has a direct impact on the lipid profile, increasing High-Density Lipoprotein Cholesterol (HDL-C) . It is a type of cholesterol found in your blood and commonly referred to as “good cholesterol”. HDL-C levels and reducing serum triglycerides, which may offer protection against atherogenic dyslipidemia, a disorder characterized by abnormal levels of lipids (fats) and lipoproteins in the blood.1
The diet's impact on hypertension and renal function can be complex. While it may not have a significant effect on blood pressure control, patients with renal insufficiency may experience increased blood pressure due to metabolic acidosis. For patients with chronic kidney disease (CKD), the ketogenic diet needs careful consideration, as it may exacerbate certain renal complications and mineral metabolism issues. Supervision by healthcare professionals is essential in such cases.
In terms of inflammation, ketone bodies have been found to modulate the inflammasome and reduce the production of pro-inflammatory molecules, suggesting a potential benefit for inflammatory conditions like atherosclerosis, which is relevant to PAD.
In summary, the low-carbohydrate ketogenic diet has the potential to address several risk factors associated with PAD, including weight management and glycemic control, as well as lipid profile improvements. However, its long-term safety and suitability for individuals with specific health conditions, such as hypertension and CKD, require careful consideration and expert guidance. More research is needed to fully understand its implications for PAD management and overall health.

- Intermittent Fasting Diet
Eating too much and thereby consuming too many calories at each meal can contribute to obesity, which worsens the condition and its associated risk factors of PAD. Intermittent fasting (IF) can help gain significant weight loss by limiting eating time and extending overnight fasting. This has positive effects on PAD and its related health problems.
Initially, the benefits of IF were thought to be mainly focused on weight loss, raising concerns about its safety and effectiveness for people with other health issues, regardless of weight loss. “Human studies show promise for cardiovascular benefit in intermittent fasting. Although the exact mechanisms remain to be elucidated, intermittent fasting appears to positively impact multiple cardiovascular risk factors including obesity, hypertension, dyslipidemia, and diabetes.”6
Recent studies have shown that IF also plays a central role in reducing inflammation. The physiological conditions resulting from IF decreases oxidative stress, influences the gut bacteria, and regulates the immune system, all which of which helps slow down the development of atherosclerosis.1 “Recently, a central role of IF on the modulation of the inflammatory process was confirmed. IF significantly reduces oxidative metabolic stress, modulates the intestinal microbiota and regulates the activity of the immune system, contributing to the slowdown of the atherosclerotic process”.1
“Benefits from the use of the IF diet were confirmed in research on the development of atherosclerosis. Intermittent fasting inhibits the development of atherosclerotic plaque by reducing the concentration of inflammatory markers, such as IL-6, homocysteine, and CRP.”2 Fasting also improves liver function by reducing the accumulation of triglycerides, leading to better lipid metabolism and lower levels of Low-Density Lipoprotein (LDL). It is a type of lipoprotein that carries cholesterol and triglycerides (fats) from the liver to various cells and tissues in the body, and it is often referred to as “bad cholesterol”. LDL cholesterol in the bloodstream. This prevents the deposition of oxidized LDL on the arterial walls.1
IF can be a beneficial approach for most PAD patients who are not at risk of low blood sugar levels or osteoporosis, as well as those without severe obesity or excessive inflammation. However, more research is needed to fully understand the implications of IF specifically for PAD.
Although more detailed research is needed for each respective diet, personalized dietary interventions play a pivotal role in effectively managing Peripheral Arterial Disease (PAD). Among the four studied diets, a Mediterranean diet emerges as particularly suitable for PAD patients. As the disease advances to critical limb-threatening ischemia (an inadequate blood supply to a part of the body), and the possibility of amputation, it becomes crucial to focus on the patient's nutritional status, address any deficiencies, and take measures to prevent excessive weight gain. Incorporating regular evaluations of diet and eating habits into the PAD treatment plan can help reduce residual risk and improve overall outcomes. By tailoring dietary recommendations to individual characteristics, comorbidities, and personal needs, healthcare professionals can enhance the effectiveness of PAD management and foster better long-term health for patients.
September is PAD Awareness Month
Peripheral Artery Disease or PAD is a chronic circulatory condition that affects over 20 million Americans and is more common than Alzheimer’s, Stroke, and most forms of cancer. Of those diagnosed with PAD, it is estimated that 200,000 of them – disproportionately from minority communities – will suffer avoidable amputations every year. We invite you to take part in raising awareness of this devastating condition and help your friends get educated on a matter of life and limb.
- Get Social: Share because you care
Post messages and links to raise awareness on social media using the hashtags:
#PADawarenessmonth
#PADawareness
#PeripheralArteryDisease
- Post educational articles about Peripheral Artery Disease. Please share the following articles on your Facebook, Instagram, X (Twitter), or other social media pages.
Articles:
- What Is Peripheral Artery Disease?
- Peripheral Artery Disease Questions & Answers with Dr. Jaafer Golzar
- 8 Causes of Peripheral Artery Disease
Educational Resources:
- PAD Webinar – Watch an overview and treatment options for PAD
- eBook Download: Treating Peripheral Artery Disease: Restoring Flow Down to the Toes
- Download: Peripheral Artery Disease: Questions For Your Doctor
- Check Friends' and Loved-Ones' legs and feet for signs of PAD
Do they have poor circulation? Is there non-healing wounds on their legs or feet? Are there signs of gangrene? Simply removing someone’s socks can help them get the care they need.
- Letter to the Editor
If you suffer from PAD or know someone who has PAD, your local newspaper can be a great way to educate your community. You may want to encourage your doctor to write a letter as well.
- Coordinate Patient Seminar and Screening at Hospitals, Clinics, and Health Centers
Work with your local hospital, clinic, and health centers to add a PAD awareness event to their roster of community education classes and include screening to help identify undiagnosed patients.
- Get help
If you know of someone who is suffering from the symptoms of PAD, have them visit a trained physician. If you need help finding someone in your community, please visit our Find a Doctor form to find one near you.
Literature Cited
- Cecchini AL, Biscetti F, Rando MM, Nardella E, Pecorini G, Eraso LH, Dimuzio PJ, Gasbarrini A, Massetti M, Flex A. Dietary Risk Factors and Eating Behaviors in Peripheral Arterial Disease (PAD). Int J Mol Sci. 011
- Malinowski, B.; Zalewska, K.; W˛esierska, A.; Sokołowska, M.M.; Socha, M.; Liczner, G.; Pawlak-Osi´ nska, K.; Wici ´ nski, M. Intermittent Fasting in Cardiovascular Disorders-An Overview. Nutrients 2019, 13
- Le, L.T.; Sabaté, J. Beyond meatless, the health effects of vegan diets: Findings from the Adventist cohorts. Nutrients 2014, 2142
- Crowe, F.L.; Appleby, P.N.; Travis, R.C.; Key, T.J. Risk of hospitalization or death from ischemic heart disease among British vegetarians and nonvegetarians: Results from the EPIC-Oxford cohort study. Am. J. Clin. Nutr. 2013, 97, 601
- Adair, K.E.; Bowden, R.G. Ameliorating Chronic Kidney Disease Using a Whole Food Plant-Based Diet. Nutrients 2020, 12, 1007, 1
- Dong, T.A.; Sandesara, P.B.; Dhindsa, D.S.; Mehta, A.; Arneson, L.C.; Dollar, A.L.; Taub, P.R.; Sperling, L.S. Intermittent Fasting: A Heart Healthy Dietary Pattern? Am. J. Med. 2020, 6
- Estruch, R.; Ros, E.; Salas-Salvadó, J.; Covas, M.-I.; Corella, D.; Arós, F.; Gómez-Gracia, E.; Ruiz-Gutiérrez, V.; Fiol, M.; Lapetra, J.;et al. Primary prevention of cardiovascular disease with a Mediterranean diet. N. Engl. J. Med. 2013, 12-13
- Martinez-Gonzalez, M.A.; Bes-Rastrollo, M.; Serra-Majem, L.; Lairon, D.; Estruch, R.; Trichopoulou, A. Mediterranean foodpattern and the primary prevention of chronic disease: Recent developments. Nutr. Rev. 2009, S113
- Tuso, P.; Stoll, S.R.; Li,W.W. A plant-based diet, atherogenesis, and coronary artery disease prevention. Perm. J. 2015, 19, 62.